Urinary System: Functions, Anatomy, and Urine Formation
Lesson Overview
Have you ever wondered how your body naturally maintains internal balance without your conscious effort? The urinary system plays a key role in silently managing waste removal and fluid regulation. In this urinary system lesson, we'll clarify how these vital functions happen and solve common misunderstandings through easy explanations and examples.
Overview of Urinary System Functions and Organs
Here is the overview of urinary system functions and organs.
Primary Functions:
- Filtration and waste removal: Kidneys filter wastes like urea from the blood.
- Fluid and electrolyte balance: They regulate water and salt levels.
- Acid-Base Balance: Kidneys maintain blood pH.
- Blood pressure regulation: They adjust blood volume and secrete the enzyme renin.
- Hormone production: Kidneys produce erythropoietin (EPO), essential for red blood cell production.
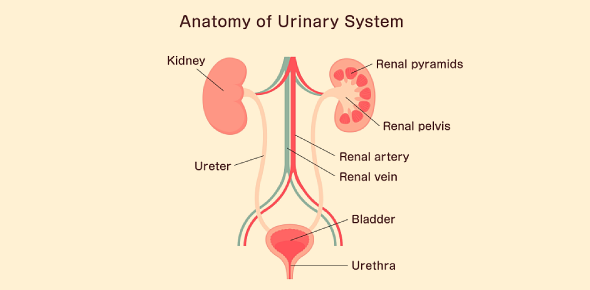
Key Organs:
- Kidneys (2): Filter blood and produce urine.
- Ureters (2): Transport urine to the bladder.
- Urinary Bladder: Stores urine temporarily.
- Urethra: Releases urine externally.
Kidney Structure: Gross Anatomy and Blood Flow
Key Structures:
- Renal cortex: Outer region; site of initial filtration.
- Renal medulla: Contains renal pyramids, essential for urine concentration.
- Renal pyramids and papillae: Collect and drain urine.
- Renal columns: Tissue separating pyramids, containing blood vessels.
- Hilum: Entry and exit point for blood vessels and ureters.
Kidney Blood Flow Pathway:
- Renal artery → Segmental arteries → Interlobar arteries
- Arcuate arteries → Cortical radiate arteries
- Afferent arterioles → Glomerular capillaries → Efferent arterioles
- Peritubular capillaries (or vasa recta) → Renal veins → Inferior vena cavaFF
The Nephron: Functional Unit of the Kidney
Each kidney has over a million nephrons, tiny structures responsible for urine production.
Nephron Structure:
- Renal Corpuscle: Includes the glomerulus (capillary network) and Bowman's capsule (captures filtrate).
- Renal Tubule: Includes the proximal convoluted tubule (PCT), loop of Henle, distal convoluted tubule (DCT), and collecting duct (CD).
Types of Nephrons:
- Cortical nephrons: Short loops, primarily in the cortex.
- Juxtamedullary nephrons: Long loops extending deep into the medulla, crucial for concentrating urine.
Juxtaglomerular Apparatus (JGA):
A feedback control area releases renin to regulate blood pressure and filtration rate.
The Process of Urine Formation
Urine formation involves three main processes: filtration, reabsorption, and secretion.
Glomerular Filtration
Blood pressure forces fluid and small molecules from blood into Bowman's capsule, creating filtrate. Cells and large proteins remain in the blood.
Tubular Reabsorption
Kidneys reclaim essential substances (water, glucose, salts) back into the blood from filtrate.
- Proximal tubule: Reabsorbs the majority of water and nutrients.
- Loop of Henle: Creates a concentration gradient to reabsorb more water.
- Distal tubule: Regulates ions and calcium levels.
- Collecting duct: Adjusts final water content, concentrating urine.
Tubular Secretion
Kidneys move unwanted substances from blood directly into filtrate, eliminating toxins, drugs, excess ions (H⁺, K⁺).
Urine Composition
Typical urine: 95% water, 5% wastes (urea, creatinine, ions).
Micturition: Urine Storage and Release
Urine travels from kidneys via ureters to the bladder for storage. When the bladder fills, sensory signals prompt urination.
Micturition Reflex Steps:
- Bladder fills, stretch receptors signal the spinal cord.
- Detrusor muscle contracts, internal sphincter relaxes involuntarily.
- External sphincter relaxes voluntarily, allowing urine flow.
Hormonal Control and Kidney Function
Hormones help kidneys regulate blood pressure, fluid balance, and red blood cell production:
- Renin-Angiotensin-Aldosterone System (RAAS): Controls blood pressure by adjusting salt and water retention.
- Antidiuretic Hormone (ADH): Conserves water, reducing urine volume.
- Aldosterone: Regulates sodium and potassium balance, increasing blood pressure.
- Atrial Natriuretic Peptide (ANP): Lowers blood volume and pressure by increasing salt excretion.
- Parathyroid Hormone (PTH): Regulates calcium and phosphate balance.
- Erythropoietin (EPO): Stimulates red blood cell production in response to low oxygen levels.
Integration and Common Questions
Common student questions and misconceptions addressed clearly:
- Why don't we urinate all filtered fluid?
Most water and nutrients are reabsorbed back into the blood. - Why is protein in urine a concern?
Indicates filtration barrier damage, signaling kidney disease. - Why is the medulla salty?
Enables water reabsorption and urine concentration through osmotic gradients. - Can we survive with one kidney?
Yes, a single kidney can compensate adequately by enlarging and adapting.
Rate this lesson:
 Back to top
Back to top
(119).jpg)