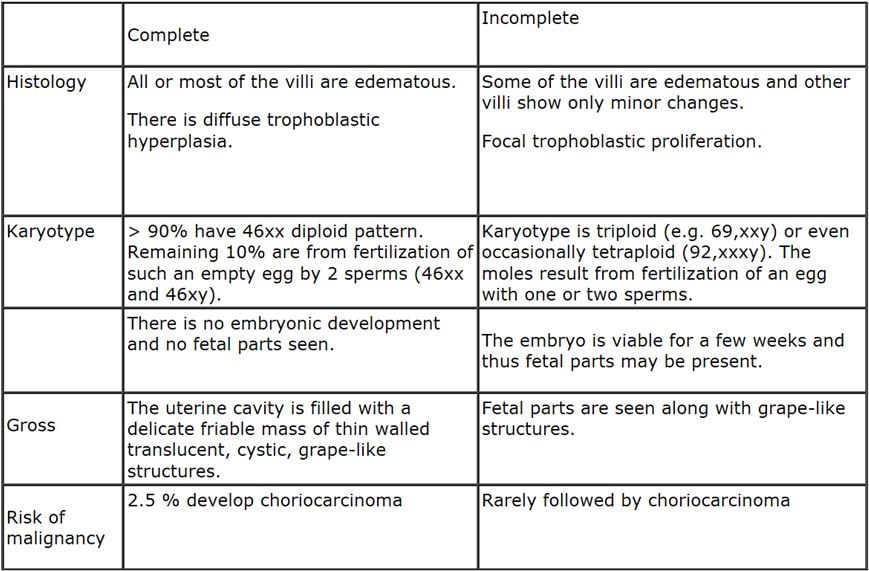
Gestational trophoblastIc disease constitutes a spectrum of tumor and tumor like conditions characterized by proliferation of pregnancy associated trophoblastic tissue of progressive malignant potential. The lesions include: Hydatidifornn mole - complete Hydatidiform mole -partial Invasive mole Choriocarcinoma Placental site trophoblastic tumor Hydatidiform mole is characterized by cystic swelling of the chorionic villi, accompanied by variable trophoblastic proliferation. The moles can occur at any age during active reproductive life, but the risk is higher in pregnant females in their teens or between the ages of 40 and 50 years. In most instances, the moles develop within the uterus, but they may occur in any ectopic site of pregnancy. This is further divided into complete type and partial type based on histologic, cytogenetic and flow cytometric studies.
In most instances, the moles develop within the uterus, but they may occur in any ectopic site of pregnancy. When discovered, generally in the 4
th or
5th month of pregnancy, the uterus is larger than the expected size for the duration of pregnancy. Most patients present with vaginal bleeding and passage of small grape-like masses. Ultrasound examination shows the typical snowstorm appearance and is diagnostic in most of the cases. The level of human chorionic gonadotrophin greatly exceeds that produced by normal pregnancy of similar period. Many studies have shown that 80-90% remain benign, 10% develop into invasive moles and 2.5% into choriocarcinoma.
INVASIVE MOLE is defined as a mole that penetrates and even perforates the uterus. There is invasion of the myometrium by hydropic chorionic villi, accompanied by proliferation of both the cytotrophoblasts and syncytiotrophoblasts. The tumor is locally destructive and invades the parametrial tissue and blood vessels. Hydropic villi may ennbolize to distant sites, such as lungs and brain, but do not grow in these organs as true metastases. It manifests clinically as vaginal bleeding and irregular enlargement of the uterus. It is always associated with persistent elevated chorionic gonadotrophin level and varying degrees of the luteinization of the ovaries. The tumor responds well to chemotherapy. Although benign, the rupture of the uterus will lead to hemorrhage.
CHORIOCARCINOMA is an epithelial malignant neoplasm of trophoblastic cells derived from any form of previously normal or abnormal pregnancy. Although most cases arise in the uterus, ectopic pregnancies provide extrauterine sites of origin. Choriocarcinoma is a rapidly growing, widely metastasizing malignant neoplasm, but once it is identified, it responds well to chemotherapy. It is preceded by several conditions; 50 % arise in hydaticliform moles, 25% in previous abortions, and 22%, in normal pregnancies and the rest in ectopic pregnancies and genital and extragenital teratomas.
The choriocarcinoma is classically a soft, fleshy, yellow white tumor with a marked tendency to form large pale areas of ischennic necrosis, foci of cystic softening, and extensive hemorrhage. Histologically, it is a purely epithelial cellular malignancy that does not produce chorionic villi and that grows by abnormal proliferation of cytotrophoblasts and syncytiotrophoblasts. The tumor invades the underlying myometrium, frequently penetrates blood vessels and lymphatics, and in some cases extends into the uterine serosa and adjacent structures. In fatal cases, the metastases are found in the lungs, brain, bone marrow, liver, and other organs. They generally present with foul smelling bloody brown discharge. The human chorionic gonadotrophin levels are elevated to the levels above those encountered in hydatidiform moles. The results of chemotherapy for gestational choriocarcinoma are spectacular and they have resulted in up to 100% cure or remssion in all patients except some whom had high-risk metastatic trophoblastic disease.
PLACENTAL SITE TROPHOBLASTIC TUMOR is a rare tumor characterized by proliferation of trophoblastic cells penetrating deep into the nnyometrium by intermediate trophoblastic cells. These cells are mononuclear and larger than cytotrophoblasts and have abundant cytoplasm. In contrast to the syncytiotrophoblasts, which produces human chorionic gonadotrophin, these cells are immune reactive to human placental lactogen. They are characterized by the absence of cytotrophoblasts and low levels of human chorlonic gonadotrophin. They are locally infiltrating but rarely may cause metastasis.



















