Why is extubating a patient in Stage II not desirable?
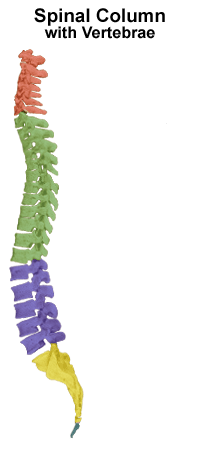
What portion of the spinal vertebrae are pictured in green?
What should be included in your report to the PACU nurse?
The aldrete score of a patient who can move all extremities, able to...
Identify 3.
What should you choose for reversal of benzodiazepine sedation?
What is the difference when doing a spinal vs epidural?
During which stage of anesthesia would a patient be at increased risk...
Optimal depth of anesthesia will maintain the BIS Number…
What would be the best choice for induction of a 5 yr male undergoing...
What portion of the spinal vertebrae are pictured in red?
What is the preferred positioning of the patient for administration of...
On which of the following patients would you consider using rapid...
What is the most frequently used method of anesthesia induction in...
During general anesthesia, we should try to maintain the patient at...
During anesthesia what leads would be most appropriate to choose to...
MAC patients should be arousable.
The Goals of any MAC case in include all of the following except:
Why are spinals inserted at a precise level in the lumbar spine?
You are the SRNA up on the OB floor today and are in the process of...
General anesthesia includes all of the following except:
What would be an appropriate induction plan for a patient with an...
You have just extubated Mr. Woo, and he begins to have a laryngospasm....
Where you expect the Spinal Cord to end on an adult patient?
You have just performed spinal anesthesia and find your patient has...
You are the SRNA for Mrs. Green who is having removal of a foriegn...
The main difference between conscious sedation and deep sedation is
Which of the following statements is false:
What would be an appropriate BIS value to maintain during maintenance...
If you were to apply a BIS monitor to yourself RIGHT NOW, what would...
The critical flaws when providing a MAC case is failure to consider...
MAC cases are easier than General cases because the patient is...
Why can a higher dose of local anesthetics be given when using...
Which of the following cases would be inappropriate for MAC...
At what level should Spinal Anesthesia be performed?
Identify 2.
CVP monitoring is most frequently used...
The primary site of action for both spinal and epidural anesthesia is...
You are attemtping to give spinal anesthesia, where do you want to...
During which level of anesthesia induced depression would your patient...
What portion of the spinal vertebrae are pictured in blue?
Identify 1.
When using the midline technique for application of spinal anesthesia...
What is the primary advantage of adding epinephrine to tetracaine for...
Decreasing consciousness increases safety risk.
You are the SRNA for Karianne, who is having her broken finger...
CSF is found in the:
If you have a hyperbaric solution (compared to CSF) and you place your...
During Stage I of Anesthesia the patient should experience all...
What is the max dose of Lidocaine plain?
You are delivering spinal anesthetic to a patient when they begin to...
You are asked to do a rapid sequence induction on a burn patient is...
What is the induction dose for Succinylcholine?
Studying for all these tests is going to cause me to have a mental...
Small controlled boluses of Propofol achieve a more consistent...
The meninge that adheres to the surface of the spinal cord...
Today you are caring for Pete, a 34 yr old male with Down’s...
Which of the following is NOT an absolute contraindication for spinal...
The most commonly selected anesthetic solution for spinal anesthetic...
What BIS reading would you expect to see in a patient in Stage IV...
What is the induction dose for Versed?
Which of the following is NOT one the goals during maintenance of...
What do you predict will be the effect of intubation on BIS, BP...
How would you reverse the effects of hypnotic agents?
At which BIS value would you see an isoelectric EEG?
Which of the following will cause an increase in MAC requirements?
After performing Spinal anesthesia you have a Sensory blockade at the...
Some indications for extubating someone deep include all of the...
Which of the following drugs would not be appropriate to use during a...
Lidocaine 1% is equivalent to how many milligrams per ml?
During which stage of anesthesia would the patient experience loss of...
You are going to do a MAC case with propofol infusion on a case today....
You have just performed spinal anesthesia and found you have a motor...
What is the induction dose for Rocuronium?
At what level should epidural anesthesia be performed?
Which of the following would cause an increase in ETCO2?
Is it possible to confirm dentirogenation? If so, How?
Which of the following will not increase the risk for awareness during...
Which of the following patients is an Absolute contraindication to...
Which of the following is an advantage of epidural anesthesia over...
When properly placing a BIS monitor on a patient, where should...
Which of the following procedures CAN be performed under MAC?
The aldrete score is based on which of the following characteristics...
When properly placing a BIS monitor on a patient, where should...
You are preparing for induction of Mr. Optimus Prime. He is 6’0”...
You are caring for Fat Albert today who has a past history of...
You have just performed spinal anesthesia and found you have a...
Which of the following local anesthetics would be the best choice for...
The induction dose of Propofol is?
What is the max dose of Bupivicaine with Epi?
When would you consider using the 'loss of resistance' technique?
According to lecture, the 3 faces of MAC are all of the following...
The cauda equina is formed by the:
What is the duration of action for lidocaine when used as a spinal...
Which of the following is one of the MOST important factors that will...
Which of the following would NOT be respiratory sign that your...
Which needle would have the lowest risk of post-dural headache?
Factors that affect Fa (alveolar) include all of the following except...
During induction, the level of anesthesia-induced depression which is...
The benefits of using BIS monitoring do NOT include which of the...
Factors that affect Uptake include all of the following except:
The aldrete score of a patient who is unable to move any extremities,...
Which of the following BEST describes the BIS number?
How will administration of methylene blue affect pulse oxymetry?
The aldrete score of a patient who can move 2 extremities, able to...
You are looking at pressure readings on your vent because you are...
You are caring for Ms. UglyFoot who is in the OR today having a...
You are performing an epidural on a patient in labor, would you expect...
According to lecture, why are inhalation anesthetics potentially the...
When using the paramedian technique for application of spinal...
Which of the following is an advantage of spinal anesthesia over...
You are the SRNA for a 4 yr old female. Where would you expect her...
During emergence, the patient will typically become responsive and...
You are giving lidocaine IV prior to administration of propfol on a...
You are the SRNA for a pt undergoing a minor procedure today. Your...
During maintenance of anesthesia, where should your arterial BP and...
When performing an epidural on a patient whose ligamentum flavum is...
The posterior or dorsal root ganglion contains:
What is the Aldrete score for an anesthetized patient, who is...
Which of the following decreases MAC? (more than one answer)
Which of the following drugs would you be MOST cautious about when...
All of the following are factors that affect the level of spinal...
Induction of anesthesia is characterized by…. (two answers)
Diastolic BP is usually lower with automated devices than with direct...
When giving spinal anesthesia it is considered ________ to add...
According to our handout, what is clinical anesthesia?
Where would you expect the spinal canal to end on an adult patient?
Which layer of of the spinal meninges is most impermeable to drugs?