Coordination Of Dual Eligible Services
-
Check all that apply: Medicare is a federal health insurance program for
-
People with disabilities who have been receiving Social Security Disability Insurance (SSDI) for more than 24 months
-
People 65 or older
-
Healthy children that need medical coverage
-
People with End-Stage Renal Disease
-
Individuals diagnosed with Amyotrophic Lateral Sclerosis (ALS), commonly known as Lou Gehrig's Disease
-
This quiz assesses knowledge on Medicare and dual eligibility coordination, covering Medicare Parts, eligibility, and cost-sharing aspects. It is crucial for professionals managing healthcare services for dual eligible individuals.
Quiz Preview
- 2.
What does Medicare Part D cover?
-
Inpatient hospital stay
-
Prescription Drugs
-
Preventive Services
-
Doctor's Visits
Correct Answer
A. Prescription DrugsExplanation
Medicare Part D covers prescription drugs. This means that it helps to pay for the cost of prescription medications that individuals need to manage their health conditions. It is a separate part of Medicare that can be added to Original Medicare or included in a Medicare Advantage plan. Medicare Part D plans are offered by private insurance companies and provide coverage for a wide range of prescription drugs, including both generic and brand-name medications. The coverage provided by Medicare Part D can help individuals afford the medications they need to stay healthy and manage their medical conditions.Rate this question:
-
- 3.
Original Medicare is Medicare services covered through a Medicare plan. True or False?
-
True
-
False
Correct Answer
A. FalseExplanation
The statement is incorrect. Original Medicare refers to the traditional Medicare program, which includes Part A (hospital insurance) and Part B (medical insurance). It does not include any specific mention of Medicare services covered through a Medicare plan. Therefore, the correct answer is False.Rate this question:
-
- 4.
Medicare Part C is
-
A Medicare Advantage Plan that covers both Medicare Part A and Part B insurance benefits.
-
Medicare that covers prescriptions only.
-
Medicare that covers only inpatient hospital stay.
-
Medicare that covers preventative services only.
Correct Answer
A. A Medicare Advantage Plan that covers both Medicare Part A and Part B insurance benefits.Explanation
Medicare Part C, also known as a Medicare Advantage Plan, provides coverage for both Medicare Part A and Part B insurance benefits. This means that it includes hospital insurance (Part A) and medical insurance (Part B) coverage. Unlike other options listed, Medicare Part C is not limited to prescriptions, inpatient hospital stays, or preventative services only. It offers a comprehensive package of benefits that combines both Part A and Part B coverage.Rate this question:
-
- 5.
People that receive Medicare may be responsible for cost sharing, which may include
-
Monthly premium payments.
-
Co-pays.
-
Coinsurance.
-
Deductibles.
-
All of the above.
Correct Answer
A. All of the above.Explanation
Medicare is a government health insurance program in the United States that provides coverage for individuals who are 65 years old or older, as well as certain younger individuals with disabilities. While Medicare covers a significant portion of healthcare costs, it does not cover everything. Therefore, people who receive Medicare may be responsible for cost sharing, which includes various types of payments. This can include monthly premium payments, co-pays (a fixed amount paid for certain services), coinsurance (a percentage of the cost of services), and deductibles (a set amount that must be paid before Medicare coverage begins). Therefore, the correct answer is "All of the above" as all of these forms of cost sharing may be applicable for Medicare recipients.Rate this question:
-
- 6.
Medicare beneficiaries who qualify to receive all Medicaid services are called
-
Medically Needy.
-
Full Benefit Dual Eligibles.
-
Qualified Medicare Beneficiaries.
-
Partial Duals.
Correct Answer
A. Full Benefit Dual Eligibles.Explanation
Full Benefit Dual Eligibles refers to Medicare beneficiaries who qualify to receive all Medicaid services. This means that they are eligible for both Medicare and Medicaid and can access a comprehensive range of healthcare services covered by both programs. The term "Full Benefit" signifies that these individuals have access to the full range of benefits provided by both Medicare and Medicaid.Rate this question:
-
- 7.
The QMB Program
-
Allows qualified individuals to have Medicaid pay Medicare for Medicare Part B premiums.
-
Allows qualified individuals the option to enroll into Medicaid Managed Care Plans outside of their region.
-
Allows qualified individuals to have Medicaid pay for their Medicare premiums, deductibles, and coinsurance.
-
Allows qualified individuals the option to hire a family member to help provide services in the home.
Correct Answer
A. Allows qualified individuals to have Medicaid pay for their Medicare premiums, deductibles, and coinsurance.Explanation
The QMB Program allows qualified individuals to have Medicaid pay for their Medicare premiums, deductibles, and coinsurance. This means that individuals who meet the eligibility criteria can receive financial assistance from Medicaid to cover the costs associated with their Medicare coverage, including premiums, deductibles, and coinsurance. This can help alleviate the financial burden for those who may struggle to afford these expenses on their own.Rate this question:
-
- 8.
The SLMB Program
-
Allows qualified individuals to have Medicaid pay Medicare for Medicare Part B premiums.
-
Allows qualified individuals the option to enroll into Medicaid Managed Care Plans outside of their region.
-
Allows qualified individuals to have Medicaid pay for their Medicare premiums, deductibles, and coinsurance.
-
Allows qualified individuals the option to hire a family member to help provide services in the home.
Correct Answer
A. Allows qualified individuals to have Medicaid pay Medicare for Medicare Part B premiums.Explanation
The SLMB Program allows qualified individuals to have Medicaid pay Medicare for Medicare Part B premiums. This means that individuals who meet the eligibility criteria can have their Medicare Part B premiums covered by Medicaid, reducing their out-of-pocket expenses for healthcare. This program helps to ensure that low-income individuals have access to necessary medical services without the burden of high premium costs.Rate this question:
-
- 9.
If a recipient has Medicare and Medicaid, Medicare is the primary insurance.
-
True
-
False
Correct Answer
A. TrueExplanation
If a recipient has both Medicare and Medicaid, Medicare is considered the primary insurance. This means that Medicare will be the first insurance to pay for any medical services or treatments that the recipient receives. Medicaid, on the other hand, will act as the secondary insurance and will cover any remaining costs that Medicare does not cover. This is because Medicare is generally available to individuals who are 65 years or older, while Medicaid is a government program that provides healthcare coverage to low-income individuals and families. Therefore, Medicare takes precedence over Medicaid in terms of coverage.Rate this question:
-
- 10.
If a member has Medicare and a MMA Plan, and wants to know who is going to cover their services, the agent should advise the member that
-
They will need to contact AHCA for help with determining which insurance is going to cover their services.
-
They should contact the MMA plan's case manager. The MMA plan is responsible for coordinating the member's care with Medicare and ensuring that the MMA plan does not authorize or provide duplicative services.
-
They can just give all of their health plan cards to the provider they are seeing and let them figure it out.
-
They need to contact Medicare to determine what they don't cover and compare that information to what the MMA plan does cover.
Correct Answer
A. They should contact the MMA plan's case manager. The MMA plan is responsible for coordinating the member's care with Medicare and ensuring that the MMA plan does not authorize or provide duplicative services.Explanation
The correct answer is to advise the member to contact the MMA plan's case manager. The MMA plan is responsible for coordinating the member's care with Medicare and ensuring that the MMA plan does not authorize or provide duplicative services. This means that the case manager will be able to provide the member with the necessary information regarding who will cover their services and prevent any duplication of services.Rate this question:
-
- 11.
Susan has Medicare and Medicaid. She wants to know which MMA plan is affiliated with her Medicare plan. How should the agent proceed?
-
Refer Susan to Medicare.
-
Advise Susan which MMA plans sounds similar to the Medicare plan she has.
-
Refer Susan to the AHCA Medicaid Helpline.
-
Advise Susan to contact the Social Security Administration to obtain a list of MMA plans affiliated with Medicare plans.
Correct Answer
A. Refer Susan to Medicare.Explanation
Since Susan has both Medicare and Medicaid, the agent should refer her to Medicare to find out which MMA plan is affiliated with her Medicare plan.Rate this question:
-
- 12.
According to the eligibility information in the hover, this recipient would be __________ for MMA.
-
Mandatory
-
Voluntary
-
Excluded
Correct Answer
A. ExcludedExplanation
Based on the eligibility information provided in the hover, the recipient would be excluded from MMA.Rate this question:
-
- 13.
Barbara states she needs to know who is going to cover her inpatient stay for her surgery coming up next month. Barbara has Medicare and Better Health for her MMA Medicaid plan. What information should be provided to Barbara?
-
Advise Barbara that she has Better Health on file and they will cover the services.
-
Inform Barbara, that since she has Medicare, Better Health will not cover anything for her.
-
Advise Barbara to contact Better Health to determine how the services are going to be covered.
-
Tell Barbara to call the Social Security Administration to find out who is going to cover services.
Correct Answer
A. Advise Barbara to contact Better Health to determine how the services are going to be covered.Explanation
Barbara should contact Better Health to determine how her inpatient stay for her surgery will be covered. This is because Better Health is her MMA Medicaid plan, and they will have the information regarding coverage for her specific healthcare services. It is important for Barbara to verify with Better Health to ensure that her surgery expenses will be taken care of.Rate this question:
-
- 14.
Flora says she received a letter saying she is Medicaid eligible and she wants to choose a plan. She has been advised that the type of Medicaid she has will not allow her to enroll into a plan. Flora wants to know what kind of Medicaid she has and what she needs to do about health coverage. What information should be provided to Flora?
-
Tell Flora, she can't choose a plan and discontinue the call.
-
Submit a discrepancy log to request for Flora to be enrolled into a plan.
-
Advise Flora that Medicare is her primary insurance and she has limited Medicaid coverage that picks up some of the out of pocket expenses from Medicare.
-
Advise Flora that she can't pick a plan because she has FFS.
Correct Answer
A. Advise Flora that Medicare is her primary insurance and she has limited Medicaid coverage that picks up some of the out of pocket expenses from Medicare.Explanation
The correct answer is to advise Flora that Medicare is her primary insurance and she has limited Medicaid coverage that picks up some of the out of pocket expenses from Medicare. This information is important for Flora to understand her current health coverage situation and what expenses are covered by Medicaid. It also helps her make informed decisions about her healthcare needs and options.Rate this question:
-
- 15.
Irene states she has Medicare and Medicaid. She wants to know who should be covering her doctor's visit today. What information should be provided to Irene?
-
Inform Irene that Medicare will be primary and her Medicaid will be secondary.
-
Advise Irene to contact Medicare to determine how services will be covered. Inform Irene that the type of Medicaid she has does not cover services and refer her to DCF for more information on her Medicaid coverage.
-
Tell Irene that her services will be covered by straight Medicaid.
-
Advise Irene that she does not have coverage to receive any services.
Correct Answer
A. Advise Irene to contact Medicare to determine how services will be covered. Inform Irene that the type of Medicaid she has does not cover services and refer her to DCF for more information on her Medicaid coverage.Explanation
Irene should be advised to contact Medicare to determine how her doctor's visit will be covered. Additionally, she should be informed that the type of Medicaid she has does not cover services, and she should be referred to the Department of Children and Families (DCF) for more information on her Medicaid coverage. This suggests that Irene's Medicaid will likely be secondary to Medicare for her doctor's visit.Rate this question:
-
Quiz Review Timeline (Updated): Mar 21, 2023 +
Our quizzes are rigorously reviewed, monitored and continuously updated by our expert board to maintain accuracy, relevance, and timeliness.
-
Current Version
-
Mar 21, 2023Quiz Edited by
ProProfs Editorial Team -
Apr 07, 2015Quiz Created by
AHSFLTrainer
2015 Rocky Mountain Health Plans
The 2015 Rocky Mountain Health Plans quiz evaluates knowledge on RMHP as a Medicare Cost Plan, including coverage specifics like worldwide emergency care and out-of-pocket...
Questions:
40 |
Attempts:
437 |
Last updated:
Mar 20, 2023
|
2015 Health Alliance - IL Private Exchange Exam - Medicare
This 2015 Health Alliance - IL Private Exchange Exam for Medicare assesses knowledge on various plan features including CMS Star Ratings, pharmacy copayments, and member rights....
Questions:
15 |
Attempts:
1245 |
Last updated:
Mar 20, 2023
|
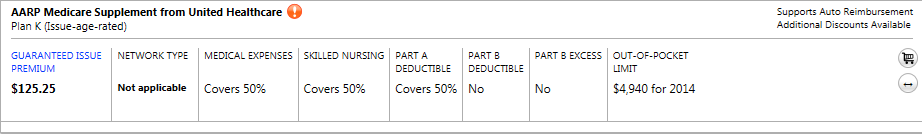
2014 - QM - Medigap Benefits
This quiz assesses knowledge on Medigap benefits, specifically focusing on Plan N, Plan K, Plan F, and High Deductible Plan F. It evaluates understanding of required disclosures,...
Questions:
10 |
Attempts:
246 |
Last updated:
Mar 21, 2023
|
WebEx Load Insurance Secondary To Medicare
This quiz focuses on loading secondary insurance to Medicare in WebEx, covering essential steps like identifying subscriber details, setting policy types, and understanding...
Questions:
6 |
Attempts:
102 |
Last updated:
Feb 23, 2024
|
Medicare: ESRD Entitlement Quiz
This Medicare: ESRD entitlement quiz assesses knowledge on End-Stage Renal Disease (ESRD), covering terminology, stages, causes, treatment options, and insurance coordination. It...
Questions:
5 |
Attempts:
167 |
Last updated:
Jan 17, 2024
|
MEDICARE/CMS AND HYPERBARIC OXYGEN THERAPY QUIZ
This quiz is a familiarization quiz on Medicare and hyperbaric oxygen therapy. Good luck!!!
Questions:
16 |
Attempts:
993 |
Last updated:
Mar 21, 2023
|
 Back to top
Back to top