Reproductive System: Hormones, Fertility, and Development Processes
Lesson Overview
- What Is the Reproductive System and Why Is It Important to Study?
- What Term Refers to a Woman Who Is Pregnant and How Is It Used?
- What Are the Signs and Hormones That Confirm Pregnancy?
- Where Does Fertilization Take Place and How Is Pregnancy Initiated?
- What Is Placenta Previa and What Are Its Clinical Implications?
- How Is the APGAR Score Used to Evaluate Newborns?
- What Are T.O.R.C.H. Infections and Why Are They Monitored During Pregnancy?
- What Are Braxton Hicks Contractions and How Do They Differ from True Labor?
- What Physiological Changes Occur During the Antepartum Period?
- Where Does Spermatogenesis Take Place and What Cells Support It?
- What Is a Bicornuate Uterus and How Does It Affect Reproduction?
- When Does Ovulation Occur and How Is It Regulated?
- Which Germ Layers Give Rise to Major Body Structures?
- What Ducts Contribute to Male Reproductive Tract Formation?
- How Is the APGAR Score Interpreted in Clinical Practice?
- What Is the Role of the Acrosome in Fertilization?
Students often find the reproductive system overwhelming, especially when connecting anatomy with hormones and clinical signs. This reproductive system lesson simplifies that complexity. It clarifies fertilization, pregnancy, and fetal development while equipping learners to handle real-world scenarios like APGAR scores, prenatal care, and reproductive disorders with confidence.
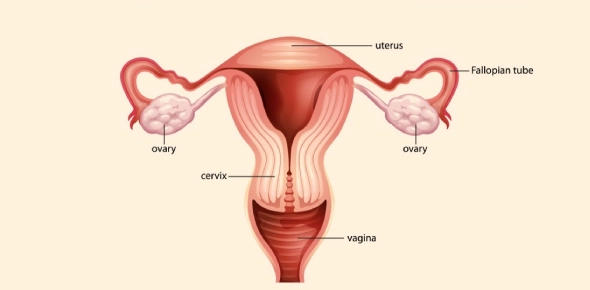
What Is the Reproductive System and Why Is It Important to Study?
Many students studying human biology struggle to understand the interconnected processes that allow human reproduction to occur. This section introduces the structure and function of both the male and female reproductive systems and highlights their importance in life sciences and health care.
- The reproductive system enables gamete production, fertilization, hormone regulation, fetal development, and childbirth.
- In females, it supports ovulation, implantation, pregnancy, and lactation.
- In males, it governs spermatogenesis, semen production, and delivery mechanisms.
Understanding the reproductive system is essential for addressing infertility, managing pregnancy, preventing diseases, and supporting maternal and neonatal health.
What Term Refers to a Woman Who Is Pregnant and How Is It Used?
Medical professionals use precise terminology to describe pregnancy history. This section explains key obstetric terms.
- The term gravida describes a woman who is or has been pregnant, regardless of the pregnancy outcome.
- Nulligravida refers to a woman who has never been pregnant.
- Primigravida refers to a woman who is pregnant for the first time.
- Multigravida refers to a woman who has been pregnant more than once.
| Term | Definition |
|---|---|
| Gravida | Any pregnancy, current or past |
| Parity | Number of pregnancies reaching viable gestational age |
| Abortus | Number of pregnancies ending in loss before viability |
These terms are essential for assessing obstetric history and guiding clinical decisions.
What Are the Signs and Hormones That Confirm Pregnancy?
Identifying early signs and hormonal markers of pregnancy is vital in clinical practice. This section explains how these signs manifest.
- Chadwick's sign is a bluish discoloration of the cervix, vagina, and vulva due to increased blood flow, seen around the sixth week of pregnancy.
- Goodell's sign is the softening of the cervix.
- hCG (human chorionic gonadotropin) is secreted by the blastocyst and maintains the corpus luteum.
- The corpus luteum secretes progesterone until the placenta assumes the role.
| Hormone | Source | Function in Pregnancy |
| hCG | Placenta (after implantation) | Maintains corpus luteum, used in pregnancy tests |
| Progesterone | Corpus luteum then placenta | Prepares and maintains endometrium |
| Estrogen | Placenta | Stimulates uterine growth, enhances blood flow |
These markers provide diagnostic and therapeutic insights during prenatal care.
Where Does Fertilization Take Place and How Is Pregnancy Initiated?
Understanding fertilization and early embryonic development is essential for reproductive biology. This section outlines the process and location.
- Fertilization occurs in the ampulla of the fallopian tube, where sperm meets and fuses with the ovum.
- The zygote undergoes cleavage and becomes a morula and later a blastocyst.
- The blastocyst implants in the uterine lining around day 6–10 post-fertilization.
| Structure | Function |
| Fallopian tube | Site of fertilization |
| Zygote | Single-cell fertilized egg |
| Blastocyst | Implants in uterus and secretes hCG |
A successful implantation triggers a hormonal cascade that supports pregnancy.
What Is Placenta Previa and What Are Its Clinical Implications?
Complications with placental placement can endanger both mother and fetus. This section explains placenta previa.
- Placenta previa refers to abnormal implantation of the placenta over or near the cervix.
- It can cause painless vaginal bleeding during the second or third trimester.
- Management depends on gestational age and bleeding severity and may include cesarean delivery.
| Type | Description |
| Complete previa | Placenta completely covers the cervical os |
| Partial previa | Placenta partially covers the cervical os |
| Marginal previa | Placenta is close to but not covering the cervix |
Recognizing and managing placenta previa is critical for safe pregnancy outcomes.
How Is the APGAR Score Used to Evaluate Newborns?
Assessment of newborns at birth is a critical part of neonatal care. This section explains how the APGAR score is used.
- The APGAR score is taken at 1 and 5 minutes after birth and evaluates 5 components: Appearance, Pulse, Grimace, Activity, and Respiration.
- Each category is scored from 0 to 2, with a maximum score of 10.
| Component | 0 | 1 | 2 |
| Appearance (skin color) | Pale or blue | Blue extremities | Pink all over |
| Pulse (heart rate) | Absent | <100 bpm | >100 bpm |
| Grimace (reflex) | No response | Grimace | Active pull away or cry |
| Activity (muscle tone) | Limp | Some flexion | Active motion |
| Respiration | Absent | Slow or irregular | Strong cry |
A score of 7–10 is considered normal; scores below 7 may indicate distress.
What Are T.O.R.C.H. Infections and Why Are They Monitored During Pregnancy?
This section discusses prenatal infections that can harm fetal development.
- T.O.R.C.H. is an acronym for Toxoplasmosis, Other infections (e.g., syphilis, varicella), Rubella, Cytomegalovirus, and Herpes simplex virus.
- These infections can cross the placenta and cause miscarriage, birth defects, or neonatal illness.
| Infection | Impact on Fetus |
| Rubella | Congenital cataracts, heart defects |
| Cytomegalovirus | Hearing loss, developmental delay |
| Herpes simplex | Skin lesions, encephalitis |
Routine screening and vaccination (where available) reduce fetal risk.
What Are Braxton Hicks Contractions and How Do They Differ from True Labor?
False labor contractions often confuse expectant mothers. This section outlines their features.
- Braxton Hicks contractions are irregular, painless contractions occurring in the third trimester.
- Unlike true labor, they do not result in cervical dilation.
| Feature | Braxton Hicks | True Labor |
| Timing | Irregular | Regular and increasing |
| Intensity | Mild, no progression | Stronger over time |
| Duration | Short, intermittent | Longer, more frequent |
| Effect on Cervix | None | Leads to dilation and effacement |
Differentiating these contractions can reduce anxiety and unnecessary hospital visits.
What Physiological Changes Occur During the Antepartum Period?
Pregnancy triggers significant systemic changes. This section explores common alterations.
- Increased urination is due to renal perfusion and uterine pressure.
- Increased respiratory demand meets oxygen needs of both mother and fetus.
- Increased basal metabolic rate (BMR) supports fetal development.
Understanding these changes helps distinguish normal from pathological symptoms.
Where Does Spermatogenesis Take Place and What Cells Support It?
This section outlines male gamete production.
- Spermatogenesis occurs in the seminiferous tubules of the testes.
- Sertoli cells nourish and support maturing sperm.
- Leydig cells between tubules secrete testosterone.
This process is continuous from puberty and is sensitive to hormonal and environmental influences.
What Is a Bicornuate Uterus and How Does It Affect Reproduction?
Structural anomalies of the uterus can affect fertility. This section describes a bicornuate uterus.
- A bicornuate uterus forms from incomplete fusion of the paramesonephric ducts.
- It is associated with recurrent miscarriage, preterm labor, and abnormal fetal positioning.
Diagnosis is often made via ultrasound or hysterosalpingography.
When Does Ovulation Occur and How Is It Regulated?
Timing ovulation is critical for conception. This section clarifies hormonal control.
- Ovulation occurs around day 14 of a 28-day cycle, during the proliferative phase.
- The LH surge from the anterior pituitary triggers ovulation.
| Hormone | Role |
| FSH | Stimulates follicle growth |
| LH | Triggers ovulation |
| Estrogen | Thickens endometrium |
Tracking ovulation aids in fertility assessment.
Which Germ Layers Give Rise to Major Body Structures?
Embryonic development involves differentiation into three germ layers.
| Germ Layer | Derivatives |
| Ectoderm | Skin, brain, spinal cord |
| Mesoderm | Bones, muscles, blood, spleen |
| Endoderm | GI tract lining, lungs, liver |
Exoderm is not a valid term and should not be confused with the legitimate germ layers.
What Ducts Contribute to Male Reproductive Tract Formation?
This section explains embryological development of male anatomy.
- Mesonephric (Wolffian) duct becomes the ductus deferens, epididymis, and ejaculatory duct.
- Development depends on presence of testosterone and Müllerian-inhibiting factor.
These structures are essential for semen transport.
How Is the APGAR Score Interpreted in Clinical Practice?
Students must learn to interpret common newborn scenarios.
- A heart rate of 80 bpm = APGAR score of 1 for pulse.
- Blue extremities with a pink torso = APGAR score of 1 for color.
Quick evaluation helps determine if resuscitation is needed.
What Is the Role of the Acrosome in Fertilization?
Fertilization requires specialized structures. This section explains the acrosome.
- The acrosome is a cap at the sperm's tip containing enzymes to penetrate the ovum.
- The acrosomal reaction allows the sperm to breach the zona pellucida and fuse with the egg membrane.
This step is critical for initiating fertilization.
Rate this lesson:
 Back to top
Back to top