Integumentary System: Layers, Functions, and Common Disorders for Students
Lesson Overview
- What Is the Integumentary System and Why Is It Essential for Human Survival?
- How Is the Integumentary System Structurally Organized?
- What Happens During Epidermal Cell Migration and Differentiation?
- What Roles Do Collagen, Elastic Fibers, and Dermal Cells Perform?
- What Is the Functional Role of the Epidermal Layers?
- What Are the Structural and Clinical Features of Burn Injuries?
- What Glands Compose the Integumentary System and What Do They Secrete?
- How Does the Integumentary System Function in Immune Protection?
- What Are the Principal Sensory Functions of the Integumentary System?
- What Types of Skin Cancer Affect the Integumentary System?
- How Do the Skin's Layers Interact During Tissue Repair?
- Why Is the Hypodermis Biologically Significant Beyond Fat Storage?
When patients suffer burns or chronic skin issues, the root often lies in gaps in understanding the integumentary system. This lesson carefully unpacks how the skin, glands, and receptors function as a protective and sensory shield. Students will grasp each layer's structure, purpose, and clinical relevance with clarity and depth.
What Is the Integumentary System and Why Is It Essential for Human Survival?
The integumentary system is a multi-functional biological barrier that plays an indispensable role in protecting the body from environmental hazards. This system includes the skin, hair, nails, sweat glands, sebaceous glands, and associated sensory receptors. The system acts as the first line of defense and supports physiological balance.
- The integumentary system provides mechanical protection against physical trauma.
- The skin regulates homeostasis through temperature control and water retention.
- The system supports immune function by housing antigen-presenting cells.
Take This Quiz:
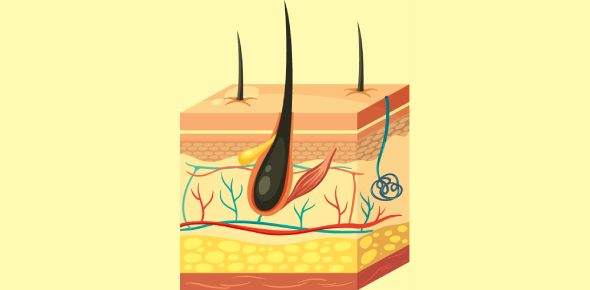
How Is the Integumentary System Structurally Organized?
The integumentary system is organized into three primary anatomical layers. Each layer has distinct tissues, cells, and functions contributing to skin physiology.
| Layer | Major Components | Key Functions |
| Epidermis | Keratinocytes, melanocytes, Langerhans cells | Protection, pigment synthesis, immune surveillance |
| Dermis | Collagen, elastic fibers, nerves, glands | Sensory reception, thermoregulation, elasticity |
| Hypodermis | Adipocytes, loose connective tissue | Insulation, cushioning, energy storage |
- The epidermis is avascular and nourished by diffusion from the dermis.
- The dermis provides structural integrity due to dense irregular connective tissue.
- The hypodermis anchors the skin to underlying muscles and bones.
What Happens During Epidermal Cell Migration and Differentiation?
Epidermal cells originate in the stratum basale and progressively migrate toward the skin surface. This journey involves biochemical changes known as keratinization.
- Keratinocytes begin in the basal layer through mitosis.
- As cells move upward, they produce keratin and form desmosomal junctions.
- Cells lose their organelles and flatten into dead corneocytes in the stratum corneum.
| Layer of Migration | Cell State Transition |
| Stratum basale | Mitotically active keratinocytes |
| Stratum spinosum | Desmosome-rich layers providing cohesion |
| Stratum granulosum | Formation of keratohyalin and lipid vesicles |
| Stratum lucidum | Clear layer in thick skin for added protection |
| Stratum corneum | Fully keratinized dead cells forming outer barrier |
- The entire epidermal turnover cycle takes approximately 28 to 40 days.
What Roles Do Collagen, Elastic Fibers, and Dermal Cells Perform?
The dermis contains fibrous proteins and specialized cells responsible for skin strength, flexibility, and immune response. This layer supports epidermal health and wound healing.
| Component | Function and Relevance |
| Collagen fibers | Provide tensile strength, resist tearing forces |
| Elastic fibers | Allow stretch and recoil, maintain normal skin tension【60†source】 |
| Langerhans cells | Act as antigen-presenting cells, detect pathogens |
| Fibroblasts | Synthesize collagen, elastin, and ground substance |
- Damage to these fibers leads to skin laxity and poor wound repair.
- Aging and UV exposure reduce collagen density and disrupt dermal integrity.
What Is the Functional Role of the Epidermal Layers?
Each layer of the epidermis is adapted to fulfill unique physiological roles. These layers work collectively to provide both a mechanical and immunological barrier.
| Layer Name | Main Function |
| Stratum basale | Proliferation of basal cells and melanocyte activity |
| Stratum spinosum | Intercellular bridges maintain structural integrity |
| Stratum granulosum | Synthesis of lipids and keratohyalin proteins |
| Stratum lucidum | Protection from mechanical stress (thick skin only)【60†source】 |
| Stratum corneum | Final barrier against desiccation and invasion |
- The stratum lucidum is present only in the palms and soles, enhancing durability.
- Loss of cohesion in these layers can result in skin disorders like psoriasis.
What Are the Structural and Clinical Features of Burn Injuries?
Burns are classified by depth, and each degree reflects progressive damage to skin layers. Understanding burn classification helps prioritize medical care.
| Degree | Affected Structures | Clinical Characteristics |
| First-degree | Epidermis | Redness, no blistering, mild pain |
| Second-degree | Epidermis + partial dermis【60†source】 | Blisters, edema, severe pain |
| Third-degree | Full-thickness epidermis + dermis | Painless necrosis, leathery texture |
| Fourth-degree | Skin, subcutaneous tissue, muscle | Charring, exposed bone, life-threatening injuries |
- Prompt cooling and sterile dressings reduce secondary damage.
- Third and fourth-degree burns require surgical grafting or debridement.
What Glands Compose the Integumentary System and What Do They Secrete?
Several glands within the skin secrete substances essential for thermoregulation, protection, and hygiene.
| Gland Type | Secretion | Functionality |
| Sudoriferous【60†source】 | Sweat | Thermoregulation, excretion of urea |
| Sebaceous | Sebum | Lubrication, antimicrobial defense |
| Ceruminous | Earwax | Traps particles, protects auditory canal |
| Mammary | Milk | Nutritional support to neonates |
- Eccrine glands are distributed widely and open to skin surface.
- Apocrine glands are confined to axillary and genital regions.
How Does the Integumentary System Function in Immune Protection?
The skin is a frontline immune organ that deploys both innate and adaptive defenses. It provides an immediate response to microbial threats.
- Langerhans cells in the epidermis detect and present antigens.
- Sebum has antimicrobial lipids and peptides that inhibit bacterial growth.
- Tight junctions between keratinocytes prevent pathogen infiltration.
| Immune Component | Function |
| Langerhans cells | Antigen capture and presentation |
| Keratinocytes | Produce cytokines and chemokines |
| Skin microbiome | Competes with pathogenic organisms |
- Disruption of immune surveillance may lead to infections and inflammatory disorders.
What Are the Principal Sensory Functions of the Integumentary System?
The skin is embedded with specialized sensory receptors that allow detection of environmental stimuli, ensuring reflexive and behavioral responses.
| Receptor Type | Stimulus Detected | Location |
| Tactile (Merkel) cells | Fine touch | Epidermal-dermal junction |
| Pacinian corpuscles | Vibration and deep pressure | Deep dermis and hypodermis |
| Meissner corpuscles | Light touch | Dermal papillae of glabrous skin |
| Ruffini endings | Skin stretch | Reticular dermis |
- These receptors contribute to proprioception and fine motor control.
What Types of Skin Cancer Affect the Integumentary System?
Skin cancer arises from uncontrolled proliferation of skin cells. Different forms vary in aggressiveness and prognosis.
| Cancer Type | Originating Cells | Characteristics |
| Basal cell carcinoma | Basal keratinocytes | Slow-growing, rarely metastasizes |
| Squamous cell carcinoma | Stratified epithelial cells | May metastasize if untreated |
| Melanoma | Melanocytes | Highly aggressive and metastatic |
- Melanoma accounts for only 1% of skin cancers but causes the majority of deaths.
- UV radiation is the leading environmental cause.
How Do the Skin's Layers Interact During Tissue Repair?
Skin wound healing involves complex biochemical signaling among different layers. This coordinated response ensures restoration of barrier integrity.
- Platelet aggregation initiates clot formation and growth factor release.
- Neutrophils and macrophages clear pathogens and debris.
- Fibroblasts in the dermis deposit new collagen fibers.
- Epidermal stem cells regenerate the superficial layers.
| Healing Phase | Cellular Events |
| Hemostasis | Clot formation, platelet activation |
| Inflammation | Infiltration by neutrophils and macrophages |
| Proliferation | Re-epithelialization, angiogenesis |
| Remodeling | Collagen alignment, scar maturation |
- Defective repair may result in chronic wounds or keloid formation.
Why Is the Hypodermis Biologically Significant Beyond Fat Storage?
The hypodermis, or subcutaneous layer, performs dynamic endocrine and structural functions beyond passive fat storage.
- Adipocytes secrete hormones like leptin that regulate energy balance.
- This layer protects internal organs from mechanical trauma.
- The hypodermis facilitates skin mobility over underlying structures.
| Hypodermal Role | Physiological Benefit |
| Thermal insulation | Maintains core temperature |
| Energy reserve | Supports metabolism during caloric deficit |
| Shock absorption | Prevents injury to muscles and bones |
- Loss of subcutaneous fat in aging or cachexia impacts systemic health.
Take This Quiz:
Rate this lesson:
 Back to top
Back to top