Male Reproductive System: Structure, Main Components, and Functions
Lesson Overview
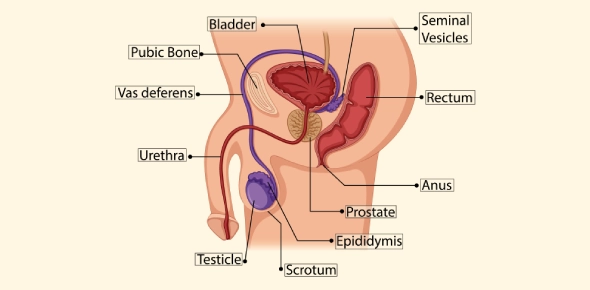
The male reproductive system is responsible for producing sperm cells and delivering them for fertilization, as well as secreting hormones such as testosterone. It consists of the primary reproductive organs (the testes) and several accessory structures and glands that support the development, maturation, and transport of sperm.
Development of the Testes
Male sex organs begin to take shape early in embryonic development. The testes (male gonads) start to differentiate from the undifferentiated gonadal tissue around the 7th or 8th week of gestation. If the embryo has a Y chromosome, a gene on it triggers this testicular development. The newly formed testes soon begin secreting testosterone, which helps direct the formation of male reproductive ducts and external genitalia.
Anatomy of the Male Reproductive System
The male reproductive anatomy includes the testes and a series of ducts and glands that produce and carry semen (the combination of sperm and supportive fluids). Key structures and their functions include:
Testes
The testes are paired oval organs housed in the scrotum (a pouch of skin below the pelvis). Inside each testis are tightly coiled seminiferous tubules where spermatogenesis (sperm production) takes place. The developing sperm cells are nourished by supportive cells within the tubules, and hormone signals (like testosterone) stimulate their production. The testes also contain interstitial (Leydig) cells that produce testosterone. Because sperm production works best at a slightly lower temperature than core body temperature, the scrotum holds the testes outside the body to keep them cooler.
Epididymis
The epididymis is a long, coiled tube attached to the back of each testis. Immature sperm from the testes move into the epididymis to mature. In the epididymis, sperm gradually gain the ability to swim (motility) and to fertilize an egg. This maturation process begins within about a day of entering the epididymis, and sperm can be stored there until ejaculation. Thus, the epididymis serves as the site of sperm maturation and storage.
Vas Deferens and Ejaculatory Duct
The vas deferens (ductus deferens) is a thick-walled muscular tube that transports mature sperm from the epididymis toward the urethra. Each vas deferens travels from the scrotum into the pelvic cavity (looping behind the bladder) and then joins with the duct of a seminal vesicle gland. This junction forms the ejaculatory duct. During ejaculation, smooth muscle contractions in the walls of the vas deferens propel the sperm forward. In the ejaculatory duct, sperm mix with the seminal vesicle fluid, and the mixture then passes through the prostate gland into the urethra.
Accessory Glands and Seminal Fluids
Several glands contribute fluids that nourish and protect the sperm, collectively forming semen when combined with the sperm cells:
- Seminal Vesicles: A pair of glands located behind the bladder that secrete a fructose-rich fluid (about 60% of semen volume) to nourish sperm. (Importantly, they secrete fructose, not glucose, as the energy source for sperm.)
- Prostate Gland: A single gland below the bladder (surrounding the upper urethra) that adds a milky, slightly acidic fluid (around 30% of semen) containing enzymes and citrate. This prostatic fluid helps to activate sperm and neutralize the vaginal environment, protecting the sperm after ejaculation.
- Bulbourethral Glands: Two small glands beneath the prostate that release a clear mucus just before ejaculation. This pre-ejaculate fluid (trace amount of the semen) lubricates the urethra and helps neutralize any residual acidity in the urethra from urine.
In addition to these glandular secretions, the sperm themselves (along with a small amount of fluid from the testes and epididymides) make up roughly 5% of the semen volume. All together, a typical ejaculation releases about 2–5 milliliters of semen. This fluid contains hundreds of millions of sperm (commonly on the order of 40 million to 600 million sperm cells per ejaculate), which increases the likelihood that at least one sperm will reach and fertilize an egg.
Penis and Urethra
The penis is the external organ that delivers semen into the female reproductive tract and also serves as the outlet for urine. It contains spongy erectile tissue (the corpus spongiosum and corpora cavernosa) that fills with blood during sexual arousal, causing an erection. The urethra runs through the center of the penis (through the corpus spongiosum) and carries semen (during ejaculation) or urine (during urination) to the outside. The urethra is surrounded and supported by subcutaneous tissue (a layer of connective tissue) and the erectile tissues of the penis. In a non-aroused state, the penis is soft and limp – this state is referred to as flaccid. During arousal, increased blood flow to the erectile tissue makes the penis firm and elevated (erect), enabling sexual intercourse and the ejaculation of semen.
Sperm Production and Pathway
The process of sperm production and their journey through the male reproductive tract involves multiple steps through specific structures. The correct order of the sperm pathway from formation to exit is outlined below:
- Seminiferous Tubules (Testes): Sperm cells are generated inside the seminiferous tubules within the testes.
- Epididymis: Immature sperm from the testes move into the epididymis, where they undergo maturation. In the epididymis, sperm gain motility (the ability to swim) and are stored until ejaculation.
- Vas Deferens: During ejaculation, sperm are propelled from the epididymis into the vas deferens. The muscular contractions of the vas deferens push the sperm upward from the scrotum into the pelvic region.
- Ejaculatory Duct: The vas deferens joins with the seminal vesicle's duct to form the ejaculatory duct. In this duct, the sperm mix with the seminal vesicle fluid as it passes through the prostate gland.
- Urethra: The ejaculatory duct empties into the urethra inside the prostate. As the semen travels through the urethra and out of the penis, it picks up the prostatic fluid and the bulbourethral mucus. The semen is then ejaculated out of the body through the tip of the penis.
Disruptions at any point in this pathway (for example, a blockage in the vas deferens) can impede the transport of sperm and thus affect male fertility.
Hormonal Control and Secondary Sexual Characteristics
The activity of the male reproductive system is regulated by hormones. The brain's pituitary gland releases follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which act on the testes. FSH stimulates the seminiferous tubules in the testes to produce sperm, while LH stimulates the Leydig cells in the testes to secrete testosterone.
Testosterone, the primary male sex hormone, has multiple crucial roles:
- It is responsible for the development of male internal reproductive structures and external genitalia during embryonic development (in the presence of a Y chromosome).
- It triggers the changes of male puberty, leading to male secondary sexual characteristics. These include growth of facial and body hair (e.g., beard, chest, pubic, and underarm hair), deepening of the voice (due to enlargement of the larynx and vocal cords), increased muscle mass and strength, and increased bone density. The testes and penis also grow larger during puberty under testosterone's influence. Testosterone additionally boosts sex drive (libido) and contributes to sperm production.
- It helps maintain adult male features and functions, such as normal sperm production, sex drive, and muscle mass.
Secondary sexual characteristics are by definition physical changes that distinguish males and females after puberty. Cognitive developments (such as improved critical thinking skills) during adolescence are not hormone-driven sex characteristics – they occur in both sexes and are not caused by testosterone. Therefore, while teenage boys do experience brain development, it is not considered a male secondary sexual characteristic, in contrast to the physical changes like body hair or voice deepening which are directly induced by testosterone.
Common Reproductive System Conditions
Prostatitis
Prostatitis is the inflammation of the prostate gland. This condition can lead to symptoms such as pelvic or lower back pain, difficulty or pain during urination, and sometimes fever. Prostatitis can be caused by bacterial infections or other factors (in some cases it is non-bacterial). In terms of terminology, prostatitis specifically refers to prostate inflammation; it is distinct from conditions like epididymitis, which is inflammation of the epididymis. Treatment for prostatitis may involve antibiotics (if bacterial) and anti-inflammatory medications, as well as supportive care.
Erectile Dysfunction
Erectile Dysfunction (ED) is the inability to achieve or maintain an erection sufficient for sexual intercourse. There are two forms:
- Primary ED: where a male has never been able to sustain an erection (this form is relatively rare).
- Secondary ED: where erectile ability was normal in the past but now has become impaired. Secondary ED is more common and can result from various causes such as stress or anxiety (psychological factors), underlying health issues that affect blood flow or nerve function (for example, cardiovascular disease or diabetes), side effects of certain medications, or other lifestyle and age-related factors.
Treatments for ED depend on the cause and severity, and can include:
- Medications: Drugs (e.g., sildenafil/Viagra, tadalafil/Cialis) that improve blood flow to the penis, facilitating an erection.
- Therapy (Sex Therapy): Counseling and behavioral techniques to reduce performance anxiety and address psychological or relationship factors contributing to ED.
- Penile Implants or Devices: For severe cases, surgical implants can be inserted into the penis to allow an erection on demand. Non-surgical vacuum erection devices (penis pumps) are another option that uses suction to draw blood into the penile tissue.
Often, a combination of medical treatments and healthy lifestyle changes (exercise, improved diet, quitting smoking, moderating alcohol) can significantly improve erectile function.
Hydrocele
A hydrocele is a condition in which excess fluid accumulates around a testicle, causing swelling of the scrotum on that side. Hydroceles are common in newborn and infant boys; they typically appear as a swollen, fluid-filled scrotum. In infants, most hydroceles are harmless and usually resolve on their own within the first year of life as the fluid is reabsorbed. In older males, a hydrocele can develop due to injury, inflammation, or infection in the scrotum. Hydroceles are usually painless, but a very large hydrocele may cause discomfort or heaviness. Treatment is not always necessary unless the hydrocele is large or persistent; in those cases, a simple surgical procedure can drain or remove the fluid.
Rate this lesson:
 Back to top
Back to top
(31).png)
(175).jpg)