|
what does a urine physical exam include |
|
-gross exam
-macroscopic |
| |
|
what are the 4 methods of urine collection |
|
-void
-manual expression
-catheterization
-cystocentesis |
| |
|
what are some advantages and disadvantages of the urine void collestion method |
|
-least traumatic
-not easiest to obtain (especially if the dog is short, if. Bassets)
-contamination is a problem
-not sterile |
| |
|
what are some advantages and disadvantages of the urine manual expression collection method |
|
-used for dogs that can't get up/walk/go to the bathroom on their own
-possibility of a bladder rupture
-potential for hematuria
-not sterile
-can have contaminates |
| |
|
what are some advantages and disadvantages of the urine catheterization collection method |
|
-can be used on dogs that can't get up
-can obtain more squamous epithelial cells due to the scraping of epithelial cells of the lower urinary tract
-relatively sterile
-decreased chance of contamination
-easy to do on males |
| |
|
what are some advantages and disadvantages of the urine cystocentesis collection method |
|
-preferred for culture
-best for microbiology
-true bladder sample
-ultrasound guided is best
-sterile if performed correctly (cleaned with surgical prep)
-remove the needle before placing in sample tube or culturette
-may need to use an ultrasound to do |
| |
|
what should you do when you have collected the urine (the amount that you collected) |
|
the quantity/volume of urine that was collected needs to be noted |
| |
|
in what type of bowl should a voided urine method be collected in |
|
a sterile bowl |
| |
|
if urine is placed in the fridge, what should you do before evaluating it |
|
let the urine come to room temperature before evaluating it
-keep some urine aside in case the doctor wants to send some out for a culture |
| |
|
how much urine do you need to collect |
|
-at least 6 mls
-ideally: 10 mls
-preferred: 12-15 mls |
| |
|
what is the most important thing when it comes to the urine collection and evaluation |
|
be consistent in your clinics |
| |
|
what can the color of urine be affected by |
|
-dyes in foods
-drugs
-blood
-hgb |
| |
|
what are the 7 different colors that urine can be |
|
-light yellow
-med yellow
-red
-brown
-orange (from drugs)
-green (from drugs)
-white (pus or UTI) |
| |
|
what are the different classifications of urine turbidity/transparency |
|
-clear
-cloudy
-flocculent
(make sure the urine is put into a clear container so it isn't mistaken for cloudy) |
| |
|
what is the normal specific gravity of urine for a dog? cat? |
|
dog: 1.001- 1.060
cat: 1.001- 1.080
(no units because it is a ratio) |
| |
|
what does the specific gravity of urine mean |
|
it is the ratio of the weight of a volume of urine to the weight of the same volume of distailled water
-it is an indicator of the concentration of dissolved material in the urine |
| |
|
what does isothenuria mean |
|
-it is when the kidneys can't form urine with a higher or lower S.G than that of protein free plasma
-it is fixed because of the damage to the nephrons
-1.008- 1.012 |
| |
|
what does it mean if the specific gravity remains the same |
|
-the kidneys are not concentrating the urine
-the urine S.G is not changing (isothenuria)
-do serial S.G checks to make sure that it is a true isothenuria |
| |
|
what can an increased specific gravity of urine mean |
|
-higher concentration of urine
-fluid loss
-dehydration
-shock
-acute renal disease
-diarrhea
|
| |
|
what can a decreased specific gravity of urine mean |
|
-chronic renal failure
-diabetes insipidus
-pyometra
-fluid overload
-diuretics |
| |
|
what does anuria mean |
|
-absence of urine
-suppression of urine formation
-ex: antifreeze patient |
| |
|
what does cystitis mean |
|
inflammation of urinary bladder |
| |
|
what does dysuria mean |
|
difficulty or painful urination |
| |
|
what does glomerular filtrate mean |
|
the fluid that passes from the blood through the glomerus |
| |
|
what does glomerular nephritis mean |
|
a form of nephritis characterized by inflammation of the renal glomeruli and no bacteris
-nephritis marked by inflammation of the glomeruli of the kidney and no bacteria |
| |
|
what does hematuria mean |
|
blood in the urine (intact RBC's) |
| |
|
what does hemoglobinuria mean |
|
hemoglobin in the urine (from lysed RBC's) |
| |
|
what does isothenuria mean |
|
a fixed S.G 1.008- 1.012 due to damage to the nephrons |
| |
|
what does myoblobinuria mean |
|
excretion of protein from the muscle breakdown in urine |
| |
|
what does nephritis mean |
|
-inflammationof the kidney
-any of various acute or chronic inflammation of the kidneys |
| |
|
what does oliguria mean |
|
-decreased urine output or volume
-seen with very dangerously low blood pressure and shock |
| |
|
what does polyuria mean |
|
-increase in urine volume
-ex: PU/PD patient will urinate large volumes |
| |
|
what does pollakuria mean |
|
-increase in frequency of urination
-ex: a blocked cat may be trying to urinate often, but only small amounts of urine comes out (straining cat) |
| |
|
what does pyelonephritis mean |
|
inflammation of kidney with bacteria |
| |
|
what does pyouria mean |
|
pus in urine (neutrophils) |
| |
|
what does glucosuria mean |
|
-blood glucose reaching the renal threshold and epinephrine release
-usually seen with diabetes mellitus (DM) |
| |
|
what does proteinuria mean |
|
-protein in the urine
-seen with strenuous exercise, hematuria and glomerular disease |
| |
|
what is the preffered time to collect a urine sample |
|
-in the morning (first urination of the day)
-it is more concentrated
-the most representative sample |
| |
|
within how much time after collecting a urine sample should it be evaluated |
|
within 30 minutes |
| |
|
if a urine sample is refrigerated, how much time can you evaluate the sample in |
|
up to 6-12 hours
-try to do a gross and chemical exam before refrigeration |
| |
|
what chemical can be used to preserve a urine sediment |
|
-a drop of formalin
-only a sediment can be preserved
-a gross and chemical exam must be done first before adding the formalin |
| |
|
what are some changes that can occur to the urine if it is allowed to sit at room temperature for to long |
|
-the urine is decomposing
-the pH changes
-the glucose decreases
-the bilirubin oxidizes
-crystals can change (they can disappear or new ones can form)
-casts can disintegrate
-amount of bacteria increases
-the RBC's can lyse |
| |
|
when performing a urine chemical evaluation, what does it mean if you see proteins |
|
-a trace can be ok
-if persistent it could be a sign of renal disease
-can be caused from hematuria, strenuous exercise or glomerular disease
-both acute and chronic renal disease can cause proteinuria
-it can be pre renal or post renal
-can also be caused from diet, drugs, sperm or anything that contains protein |
| |
|
when performing a urine chemical evaluation, what does it mean if you see ketones |
|
-found in urine when carbohydrate metabolism has been replaced with fat metabolism
-the body is unable to use carbohydrate glucose for energy so it starts using stored fat
-occurs with starvation and DKA (diabetic ketoacidotic patients)
-can be seen in unregulated diabetic cases
-ketones are a byproduct of a substance that is made when your body breaks down fat for energy |
| |
|
when performinga urine chemical evaluation, what does it mean if you see glucose |
|
-the renal threshold has been reached (170-180 BG at least has been reached)
-common reason is diabetes mellitus
-other reasons: epinephrine release, acute pancreatitis, cushing disease and stress (especially in cats) |
| |
|
when performing a urine chmeical evaluation, what does it mean when you see urobilinogen |
|
-not very accurate
-has to do with the patency of the bile duct
-more often used in human medicine
-it is a bile pigment, a product of bilirubin
-reasons: possible liver disease or hemolytic states
-greyhounds tend to have false positives |
| |
|
on a urine chemical evaluation, what can affect the pH level |
|
the pH level tends to vary depending on the diet, fever, dehydration and diabetes mellitus (DM) |
| |
|
what does acidic mean |
|
a pH less than 7 |
| |
|
what does alkaline mean |
|
a pH more than 7 |
| |
|
what does a neutral pH mean |
|
a pH of 7 |
| |
|
what can an increased protein diet do to the pH of urine |
|
it can cause an acidic pH |
| |
|
what can an increased carb diet do to the pH of urine |
|
it can cause an alkaline pH |
| |
|
when performing a urine chemical evaluation, what does it mean if you see blood (hematuria) |
|
-a few RBCs are often seen in normal dog and cat urine
-can indicate hemorrhage, uroliths, trauma, parasites, estrus or infection |
| |
|
what does it mean if you see hemoglobinuria when performing a urine chemical evaluation |
|
-it can be an intravascular hemolysi (differentiate by evaluating the sediment), heat stroke, anti-freeze, shock, AIHA, liver disease or snake venom |
| |
|
what does it mean if you see myoglobinuria when performing a urine chemical evaulation |
|
-it is the muscle breakdown
-seen in hemolytic blood diseases and bile duct obstructions
-working horses that have Monday morning disease after having a day of rest on Sunday can have myoglobinuria (their muscles show signs of wasting "Rhabdomyolysis")
-the history can be very improtant in these cases
-myoglobin is basically the oxygen carrying pigment of muscle |
| |
|
what does it mean when you see bilirubin when performing a urine chemical evaluation |
|
-it is bile pigment
-can be a sign of: liver disease, biliary obstruction
-common of liver flukes in felines (eating lizards)
-not normally seen in felines
-the threshold is higher in cats |
| |
|
what does it mean if you see nitrite during a urine chemical evaulation |
|
-normal urine contains little to no nitrite
-bacteria converts to nitrite when present in a UTI
-nitrite is the reduced form of nitrate and is not found in urine
-nitrite can be produced by some bacteria so this can be used as a screening for detection of bacteria |
| |
|
what can the odor of urine be affected by |
|
disease process |
| |
|
what are the different types of odor that urine can be |
|
-normal
-malodorous
-ammoniacel
-acetone
-strong
-pungent
-sweet (DKA)
-putrid (bad -UTI) |
| |
|
how long should urine be centrifuged for |
|
- 3 to 5 minutes
- at 1200 to 1500 rpms
-at school we do 3 minutes at 1200 rpms |
| |
|
after urine has been centrifuged, what are the two items you get in the urine tube |
|
-supernate (top portion)
-sediment (bottom portion) |
| |
|
after you have spun the urine, how do you make a urine slide to examine |
|
-pour (decant) the supernate (top portion of the urine)
-resuspend the sediment remaining in tube
-place a drop of the sediment onto a glass slide with a coverslip |
| |
|
how do you view a urine sediment on the microscope |
|
-scan on low power (10x), looking for clumps of cells and casts
-then examine on high power (40x)
-low light/ low condensor
-observe at least 10 fields
-report in #/HPF (except for crystals and bacteria) |
| |
|
if any casts are found, how should they be recorded |
|
-preferably amount seen per low power field (#/LPF) |
| |
|
how are any cells or other items found during microscopic examination of urine reported |
|
amount per high power field ( #/ HPF) |
| |
|
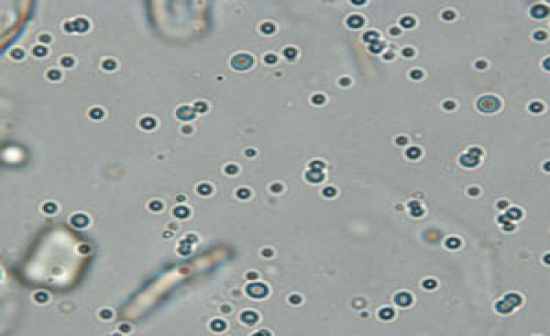
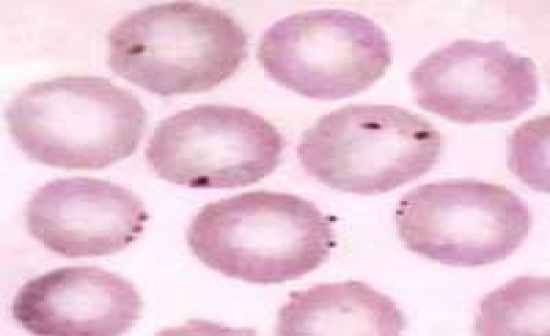
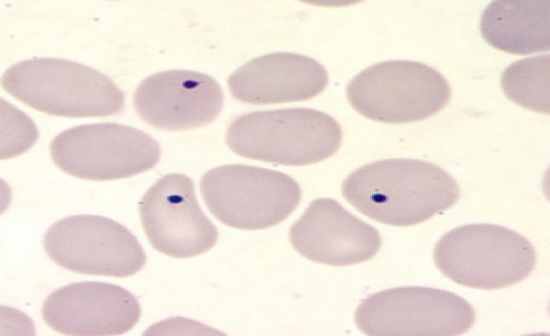
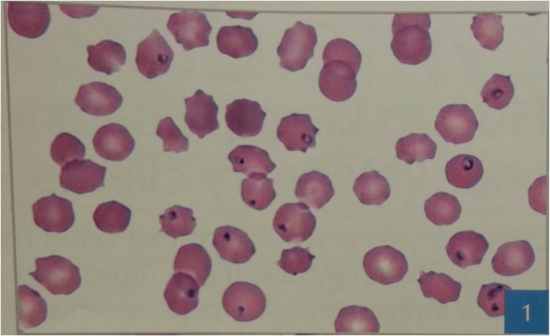
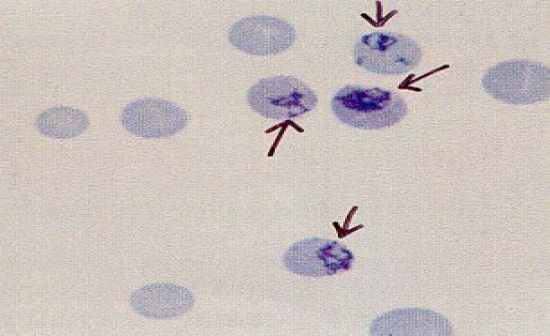
what do RBC's appear like in urine (under the microscope) |
|
-biconcave, crenated or swollen
-concentrated urine tends to have crenated cells and dilute urine has swollen RBCs |
| |
|
why might you see RBCs in urine under the microscope |
|
-they can originate from anywhere in the urinary system
-could be from cystocentesis
-could be old blood or new blood in the system |
| |
|
what is the normal amount of RBC's that should be seen in urine under the microscope |
|
-5 or less / HPF (depending on how urine was obtained)
-if seeing 5 or more /HPF, then the chemical strip should also be positive
-quantitate by # / HPF (use ranges) |
| |
|
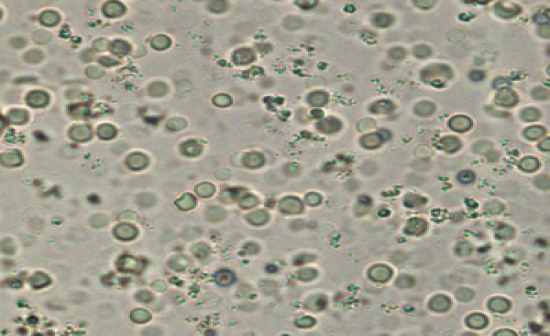
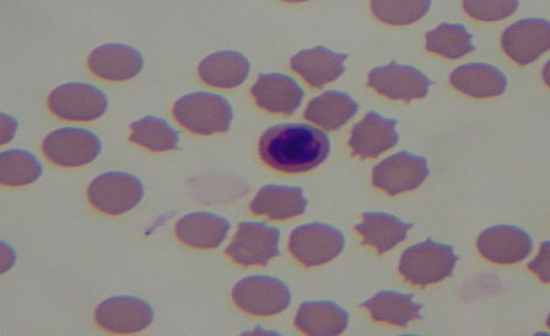
why might you see WBCs in urine under the microscope |
|
-can originate from anywhere
-you will see neutrophils (have nucleaus and granules)
|
| |
|
what is the normal amount of WBCs you will see in urine under the microscope |
|
-5 or less WBC /HPF (depending on how urine was obtained)
-quantitate by # /HPF (use ranges) |
| |
|
what does it mean if the urine has increased protein but only a few wbc's and rbc's |
|
-indicates renal issues
-can mean a glomerular problem |
| |
|
what does it mean if the urine has increased protein levels and increased rbc's and wbc's |
|
-could be inflammation in the kidneys
-inflammation of the urinary bladder
- or can be both |
| |
|
what does it mean if the urine has normal protein levels but increased rbc's and wbc counts |
|
-can indicate a UTI most likely from the bladder |
| |
|
is it normal to see epithelial cells in urine on the microscope |
|
yes, it is normal to see an occasinal epithelial cell depending on how the urine was obtained |
| |
|
what are the types of epthelial cells you may see in urine |
|
-squamous
-transitional
-renal |
| |
|
what do squamous epithelial cells look like? where do they come from? |
|
-large, flat cells
-could look like a burrito (folded, small nuclei)
-originate from the distal 1/3 of the urethra, vagina or prepuce
-primary source is the urethra
-is the largest epithelial cell |
| |
|
what do transitional epithelial cells look like? where do they come from? |
|
-smaller than squamous cells
-round to pear shaped or caudate
-have larger nucleus
-twice as big as a WBC
-always note clumping or atypical cells (very important)
-originate in the bladder or 2/3 or the urethra |
| |
|
what do renal epithelial cells look like? where do they come from? |
|
-small, round cell with large nucleaus
-larger than WBC but smaller than transitional cells
-orginate from the kidney |
| |
|
what does an increased number of renal epithelial cells indicate |
|
tubular damage |
| |
|
how should any type of cells in urine be quantitated |
|
# / HPF
-occasional, too numerous to count (tntc)
-wall to wall (w to w) |
| |
|
what should you note if you don't see any RBC's, or WBCs or epithelial cells in your urine slide |
|
don't right zero, write "none seen" (NS) |
| |
|
from smallest to largest, list the cells you will see in urine |
|
-rbc
-wbc
-renal epithelail
-transitional epithelail
-squamous epithelail
|
| |
|
what is crystalluria and what can it be caused by |
|
-it is crystals in the urine
-it is caused by the mineral compounds that make up the crystals |
| |
|
what mineral compunds make up crystals found in urine |
|
-magnesium
-ammonium
-phosphate
(these in particular make up the struvite crystal) |
| |
|
what are crystals caused by |
|
precipitation of solutes, salts and organic compounds |
| |
|
what are crystals affected by |
|
-pH
-diet
-concentration
-drugs |
| |
|
what dog breed is predisposed to having an excess amount of uric acid that leads to crystals |
|
dalmation |
| |
|
what are crystals dependent on |
|
pH |
| |
|
what crystals are most often seen in acidic urine (less than 7 pH) |
|
-calcium oxalate
-amorphous urates
-uric acid
-cystine
-tyrosine
-leucine |
| |
|
what crystalsare most often seen in alkaline urine (more than 7 pH) |
|
-triple phosphate/ struvite
-amorphous phosphate
-ammonium biurate (can be pathological)
|
| |
|
which urine crystal can be seen in al three types of pH (acidic, alkaline and neutral) |
|
calcium oxalate crystal |
| |
|
what are the most common pathologic crystals that are seen in urine |
|
-tyrosine
-leucine
-cystine |
| |
|
what can the pathologic crystals indicate |
|
liver disease |
| |
|
how are crystals found in urine quantitated |
|
- +/++/+++
- slt/few/ many
-occansonal, tntc, w to w |
| |
|
what can cause crystalluria |
|
antifreeze poisoning |
| |
|
what are the different types of casts you can find in urine |
|
-hyaline
-cellular
-granular
-waxy |
| |
|
what are casts and how are they formed? |
|
-casts are molds made of protein, clumping cells and materials with proteins
-they are formed in the lumen of the tubules of the kidney
-they are called casts because they reflect a cast of the renal tubular lumen |
| |
|
what does a hyaline cast look like and what does it mean if you see one in urine |
|
-clear, colorless, transparent
-small numbers can be seen in normal urine
-increased numbers can be significant
-the hyaline cast is where all the casts originate from |
| |
|
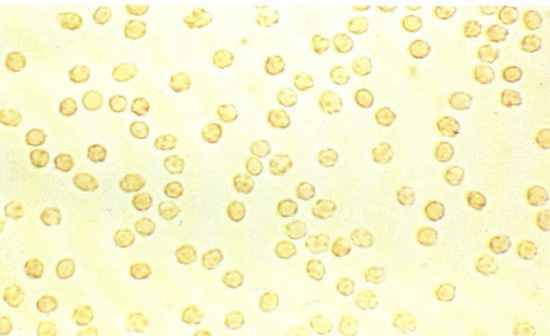
what does a cellular cast look like and what does it mean if you find one in urine |
|
-include WBC and RBC casts and fatty casts
-WBC can indicate infection or inflammation of renal tubules
-RBC can indicate renal bleeding (could be from trauma or inflammatory lesion)
-fatty can be made of fat droplets (seen more in cats with renal disease)
-epithelial casts can indicate acute nephritis
-these lead to granular casts |
| |
|
what do granular casts look like and what does it mean if you find one in urine |
|
-casts become coarse and fine granular
-start off granular and the longer they are in the kidney the more fine they become
-can indicate acute nephritis
-fine granular casts are the stage before waxy |
| |
|
what do waxy casts look like and what does it mean if you find one in urine |
|
-not very common
-have square ends
-most severe cast
-indicates chronic and severe degradation of renal tubules
-indicates chronic tubular lesions or damage
-end stage of renal disease |
| |
|
what should you do if you see a cast? a fragment of a cast? |
|
-quantite #/LPF
-if you see fragments they should be quantitated and identified |
| |
|
what is a broad cast |
|
a wide cast that can resemble any type of cast (hyaline, cellular, granular or waxy) |
| |
|
what type of bacteria can you find in urine |
|
-rod
-cocci
-chains
(report as +/++/+++) |
| |
|
what other organisms can you find in urine |
|
-yeast and other fungal organisms
-fat droplets
-sperm
-microfilaria
-parasites |
| |
|
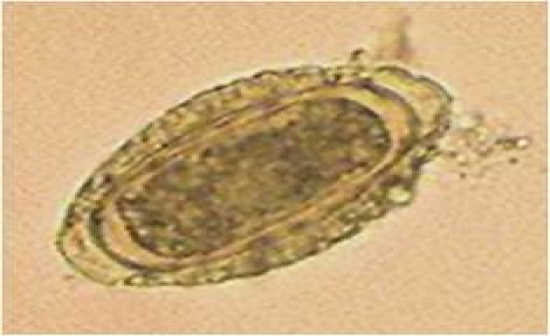
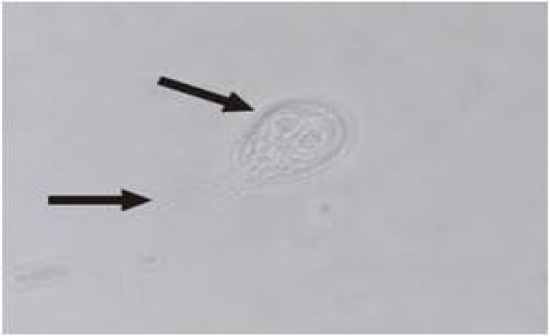
what is capillaria plica |
|
-a bladder worm ova
-ingested from eatting earth worms, food or water contaminated
-adults lay eggs in bladder and then they are passed into urine |
| |
|
what is dioctophyma renale |
|
-kidney worm ova
-transmitted from eating worms, frogs and fish
-adults inhabit the kidney, eggs passed into urine |
| |
|
what are other material (from outside the body) that can be found in urine |
|
-pollen
-debris
-hair
-parasites from outside collection (bugs) |
| |
|
what does a gross urine examination include |
|
-odor
-color
-turbidity
-S.G |
| |
|
how can you tell the difference between hematuria and hemoglobinuria |
|
spin down urine, if all the red collects at the bottom, then it is hematuria; if the urine stays red throughout, then it is hemoglobinuria |
| |
|
what are the 2 things that are quantitated by pluses (+/++/+++) when found in urine |
|
-crystals
-bacteria and sperm |
| |
|
what method of urine collection is prefered for culture and sensitivity |
|
cystocentesis |
| |
|
what does it mean if your chemstrip is positve for RBC's but know are present in the urine when evaluated |
|
you have hemoglobinuria |
| |
|
what is the S.G of distilled water |
|
1.000 |
| |
|
what indicator pads on the chemstrip are unreliable in urine |
|
-S.G
-nitrite
-leukocytes |
| |
|
what are the 4 things that make up a complete urinalysis |
|
-gross exam
-S.G
-biochemical analysis (chemstrips)
-sediment exam |
| |
|
what can clumping of transitional epithelial cells in a urine sediment indicate |
|
transitional cell carcinoma |
| |
|
what can bilirubin crystals indicate |
|
liver issues |
| |
|
in what type of pH would you see amorphous material |
|
acidic urine |
| |
|
what does pollen look like in urine |
|
-mickey mouse
-pine cone |
| |

|
|
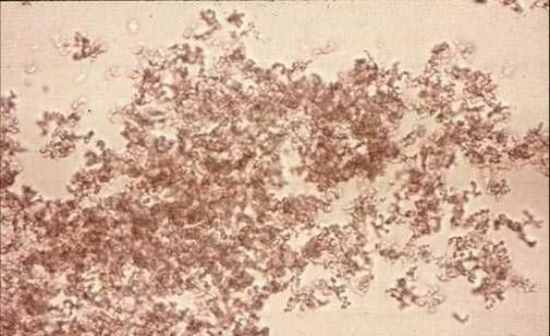
ammonium biurate |
| |

|
|
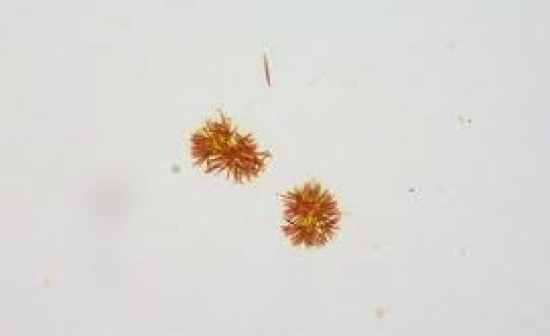
ammonium biurate (thorny apple) |
| |
|
|
amorphous urate |
| |
|
|
bilirubin crystal |
| |

|
|
calcium oxalate |
| |
|
|
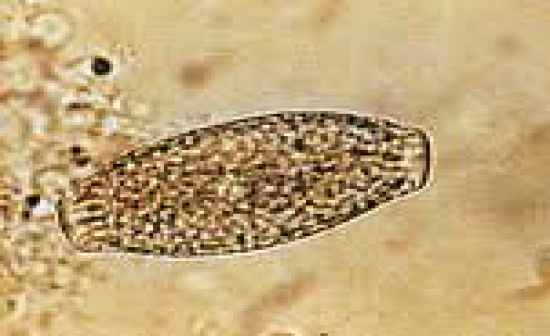
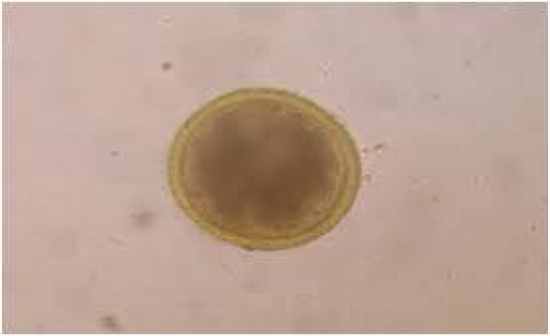
capilliaria plica |
| |
|
|
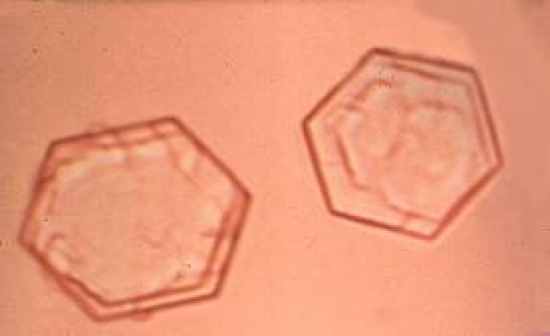
cystine |
| |
|
|
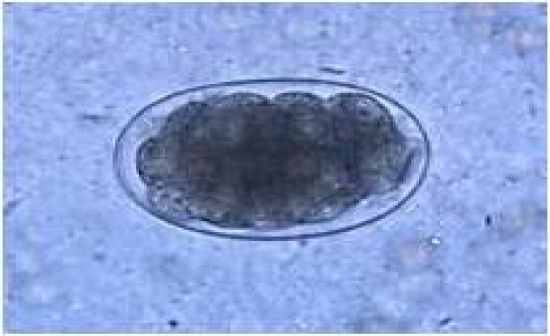
dioctophyma renale |
| |

|
|
dioctophyma renale |
| |
|
|
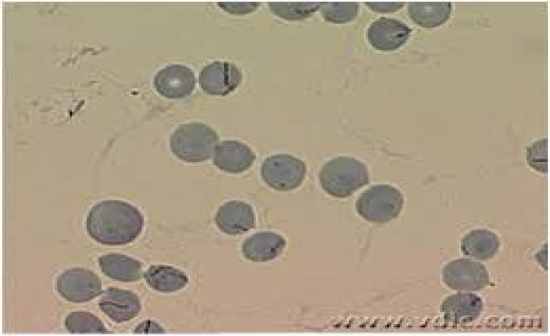
fat droplets |
| |

|
|
leucine |
| |
|
|
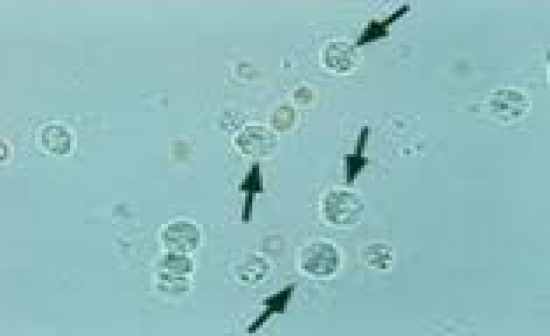
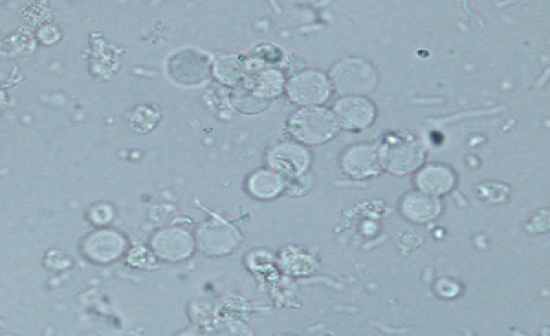
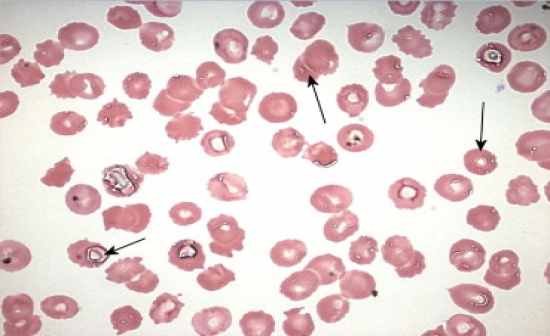
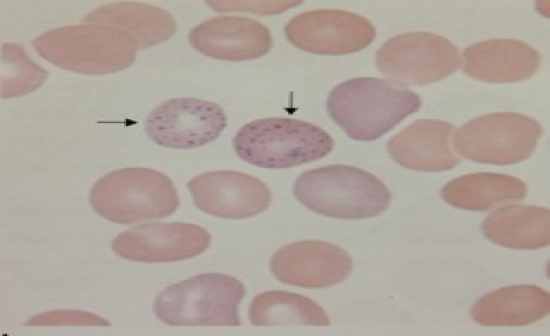
rbc's |
| |
|
|
rbc's |
| |
|
|
struvite (triple phosphate) |
| |
|
|
tyrosine |
| |
|
|
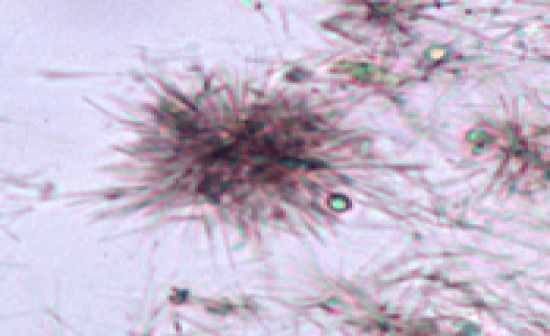
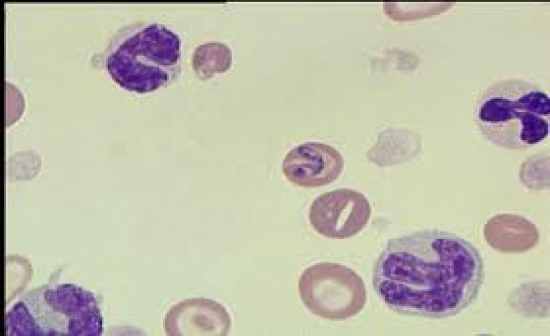
wbc |
| |
|
|
wbc |
| |
|
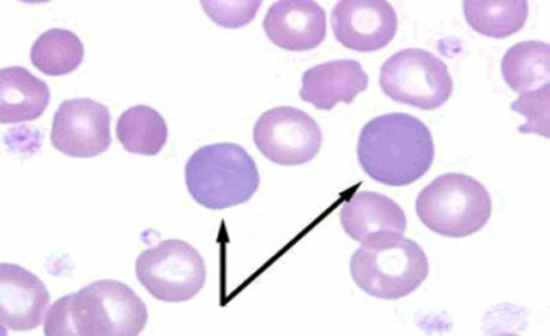
what should a normal canine RBC look like |
|
biconcave disc shaped with a central pallor |
| |
|
what should a normal feline RBC look like |
|
disc shaped with no central pallor |
| |
|
what does poikilocytosis mean |
|
a variation in cell shape (furthur identify the shape if possible) |
| |
|
what does anisocytosis mean |
|
a variation in cell size |
| |
|
what is macrocytosis and what is it a sign of |
|
-a larger than normal cell
-it is a sign of immaturity |
| |
|
what does polychromasia mean |
|
a variation in cell color |
| |
|
what does it mean if a cell has a darker color |
|
it is more immature |
| |
|
what is hypochromasia and when will you see it |
|
-it is a decreased amount of hemoglobin
-there will be an increase in size of the central pallor
-normally seen in chronic anemias |
| |
|
what are howell jolly bodies |
|
nuclear remnants in RBC's |
| |
|
what are NRBC's |
|
immature RBC with a retained nucleus |
| |
|
what is basophilic stippling and when would you see it |
|
-a RBC with many small blue dots
-you will see it in regenerative bovine blood
-also in lead poisoning in dogs/cats along with inappropriate NRBC response |
| |
|
what are heinz bodies and when would you see them |
|
-they are denatured hemoglobin
-seen in acetaminophen, vit K and toxin cases |
| |
|
what are stomatocytes and when would you see them |
|
-a RBC with a slit or mouth like clear opening
-see in dogs with chronic anemias |
| |
|
what are echinocytes and when are they seen |
|
-a cell with evenly spaced projections
-speculated RBC's
-see in crenation and rattle snake bites |
| |
|
what are acanthocytes and when are they seen |
|
-a spur cell with uneven projections
-seen in dogs with hemagiosarcomas |
| |
|
what are spherocytes and when are they seen |
|
-are small, dense, round RBC's
-seen in IMHA cases |
| |
|
what are schistocytes and when are they seen |
|
-fragmented RBC's
-seen in DIC, hemangiosarcoma and vasculitis |
| |
|
what are target cells and when are they seen |
|
-also called leptocytes and codocytes
-they have a target in the middle of the cell
-seen in a variety of conditions and in normal dogs |
| |
|
what are barr cells and when are they seen |
|
-also called leptocyte and codocyte
-have a dark bar in the middle of cell
-seen in liver disease |
| |
|
what ia a dacrocyte |
|
a tear drop shaped cell |
| |
|
what are retics and what type of stain is used to see them |
|
-retained organelles (ribosomes)
-new metheyne blue stain (supravital)
(aggregate= >5 [ more than 5] and punctate = <5 [less than 5] |
| |
|
|
humidity |
| |
|
what is another term for NRBC |
|
metarubricyte |
| |
|
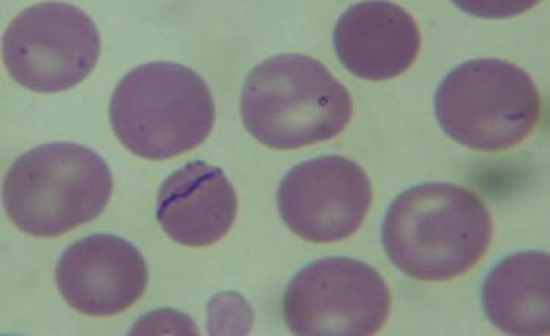
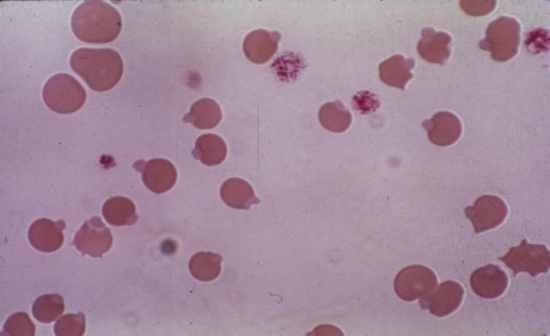
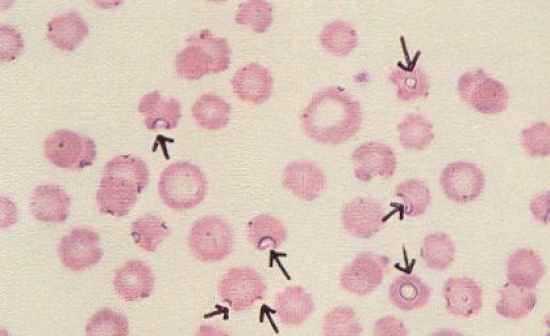
what is babesia canis and babesia gibsoni |
|
-parasites that infect RBC's and produce hemolytic anemia
-transmitted by the brown dog tick
-seen commonly in greyhounds
-tick borne disease |
| |
|
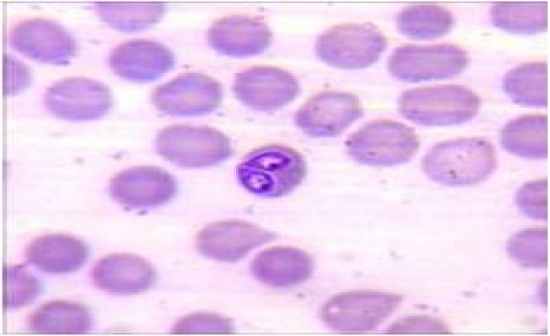
|
babesia canis |
| |
|
|
babesia canis |
| |
|
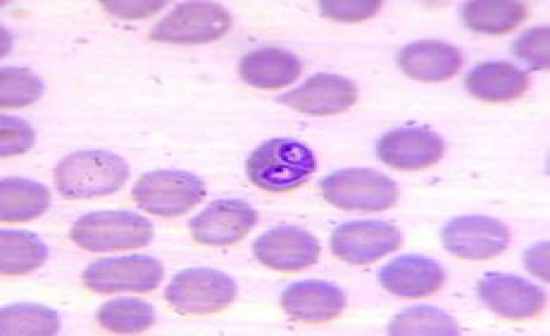
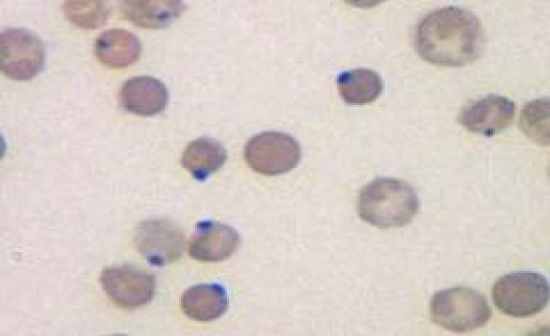
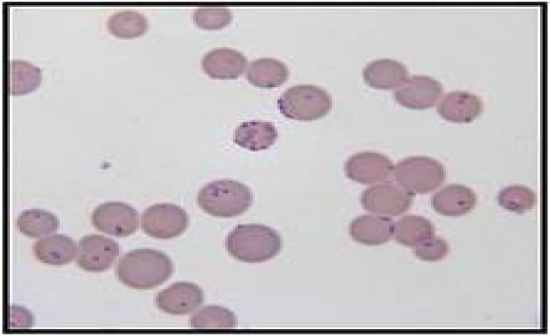
what is mycoplasma |
|
-a blood parasite also known as Hemobartonella
-it is transmitted by fleas and occasionally by ticks
-it can lead to FIA (feline infectious anemia)
-seen as rods, rings or cocci
-will fall off in EDTA
-cyclic and usually secondary (has to be tested for multiple times because you may not see it the first time you test for it) |
| |
|
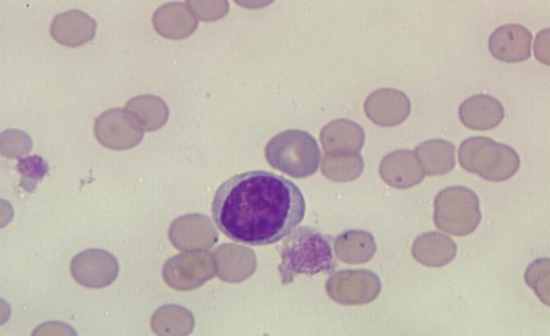
|
mycoplasma |
| |
|
|
mycoplasma |
| |
|
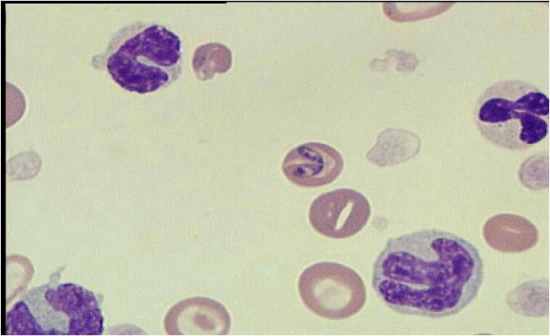
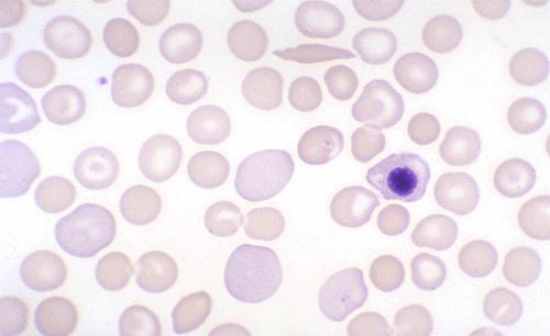
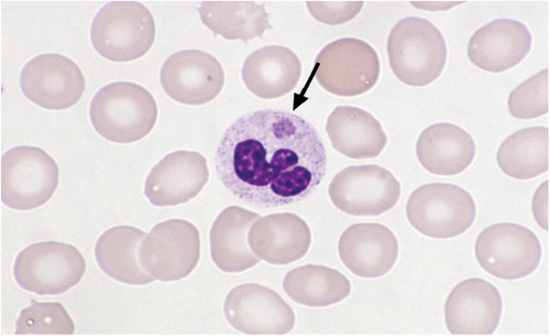
what is cytoxzoon felis |
|
-a protozoal parasite that can cause fatal disease in cats
-transmitted by the amblyomma americanum tick (lone star tick)
-seen more in big cats (tigers, cougars, etc)
-only seen in cats |
| |

|
|
cytauxzoon felis |
| |
|
if your not sure if it is rouleaux or agglutination, what should you do |
|
perform a saline agglutination test |
| |
|
what does agglutination usually mean |
|
-it is autoimmune
-indicates IMHA |
| |
|
what are distemper inclusion bodies |
|
-large aggregates of viral particles
-can form in RBC, WBC and epithelial cells |
| |
|
what is a corrected WBC count and why do we perform one |
|
-it is a formula that gives us a corrected WBC count from the machines total
-we do it when we see more than 5 NRBC's when performing a differential
-we do this because the machine is counting the NRBCs as WBC's, so we need to get an accurate WBC count
-formula: (WBC count x 100) / (100 + NRBC's counted) = corrected WBC count mm3 |
| |
|
what is anaplasma and what species does it affect |
|
-a blood parasite
-transmitted by the tick
-it affects cattle |
| |
|
what is another name for tropical pancytopenia |
|
ehrlichia canis (an inclusion found in WBC) |
| |
|
how is ehrlichia canis transmitted |
|
brown dog tick |
| |
|
what are the signs of a toxic neutrophils (DBVG) |
|
-basophilia (most indicative of toxicty)
-dohle bodies
-vacuolization (foamy)
-giantism
|
| |
|
what are some examples of degenerate neutrophils |
|
-karyorrhexis
-karyolysis
-pyknosis |
| |
|
when will you see degenerate neutrophils |
|
-often seen in tissue cytology
-not seen in peripheral blood |
| |
|
what does a reactive lymph look like (reactive cell) |
|
has a royal blue cytoplasm |
| |
|
what can cause a reactive lymph |
|
-infectious agent
-neoplasia
-immune mediated |
| |
|
what does a reactive lymph look like (plasma cell) |
|
-has an eccentric nucleus
-peri nuclear clear zone
-trailing blue cytoplasm |
| |
|
what do atypical lymph look like |
|
they have cleaved nucleus |
| |
|
what does reactive monocytes look like |
|
-intensely basophilic vacuolated
|
| |
|
what can a reactive monocyte indicate |
|
chronic inflammatory process |
| |
|
what is a left shift |
|
-immature cells
-increased number of band neutrophil |
| |
|
what is the difference between a regenerative and degenerative left shift |
|
-regen: bands with neutrophilia (increase of neutrophils)
-degen: bands with neutropenia {decrease in neutrophils} (the bands out number the segs) |
| |
|
what is a right shift |
|
- hypersegmented neutrophils
- usually due to aging
- more than 5 lobes in the cell
-can be associated with steriods |
| |
|
when does neutrophil toxicity occur |
|
-when they are released too early |
| |
|
what is a dohle bodie |
|
-a bluish cytoplasmic inclusion of a neutrophil
-made up of retained aggregates
-this is a toxic change |
| |
|
when will you have a left shift |
|
when you have an absolute count of 300 or more band neutrophils |
| |
|
what is the maturation of a erothrocyte |
|
-stem cell
-rubriblast
-prorubricyte
-rubricyte
-metarubricyte (NRBC)
-polychromatophil (retics)
-red blood cell |
| |
|
what is the maturation of a WBC |
|
-stem cell
-myeloblast
-promyelocyte
-neutrophilic myelocyte
-neutrophilic metamyelocyte
-band neutrophil
-segmented neutrophil |
| |
|
a big cell equals what |
|
an immature cell |
| |
|
why do we use saline in a direct fecal exam |
|
it is an isotonic solution which allows for movement |
| |
|
what are we looking for on a direct fecal |
|
-bacteria
-protozoa
-ova
-motility/ movement |
| |
|
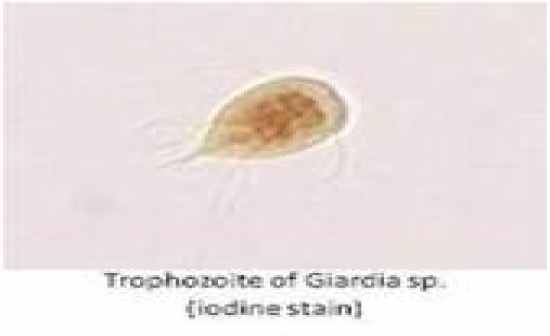
what can be seen moving on a direct smear |
|
-giardia
-motile bacteria |
| |
|
on what power do you view a direct fecal smear |
|
-scan on low
-then on high power (40x) |
| |
|
on what power do you view a fecal float on |
|
low power (10x) |
| |
|
what are you looking for on a fecal float |
|
ova |
| |
|
what are the 2 types of fecal floats and which one is preferred |
|
-standard and centrifuge
-prefer centrifuge because it forces more of the heavier eggs (ova) to rise |
| |
|
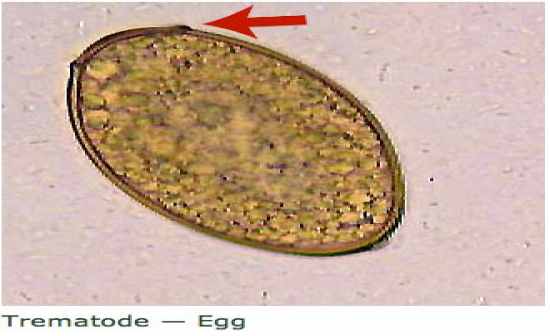
why do we do a fecal sedimentation |
|
it helps find heavier ova
-ex: liver flukes (platynossum fastosumm ova) and lung flukes |
| |
|
how long after you make a direct fecal smear should you look at it |
|
immediately |
| |
|
what is a Baermann apparatus |
|
-a large sedimentation apparatus
-used mainly for large animals to find different stages of larvae |
| |
|
what is pancreatic insufficiency |
|
-it is a maldigestion problem
-can be congenital or acquired
-the patient lacks digestive enzymes
-the patient can't dogest it's own fats, proteins and carbs |
| |
|
how do you test for pancreatic insufficiency |
|
-TLI
-trypsin like immunoassay test |
| |
|
what does the feces of a patient with pancreatic insufficiency look like |
|
-big
-greasy
-pale, greasy and voluminous |
| |
|
what power do you view a fecal sedimentation on |
|
low power (10x) |
| |
|
what power do you view fecal cytology on |
|
-scan on high power (40x)
-identify on oil |
| |
|
what is the scientific name for the hookworm |
|
ancylostoma caninum |
| |
|
what is the scientific name for the roundworm |
|
-toxocara cati
-toxocara canis |
| |
|
what is the scientific name for the whipworm |
|
trichuris vulpis |
| |
|
what are the scientific names for the tapeworm |
|
-dipylidium caninum
-taenia pisiformi |
| |
|
what is the scientific name for coccidia |
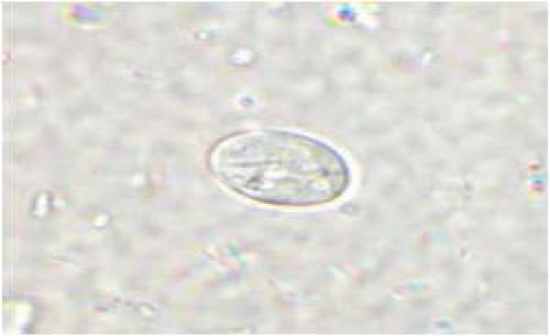
|
isospora canis |
| |
|
what solution do we prefer to use on fecals because it causes less distortion |
|
zinc sulfate solution |
| |
|
how is a standard fecal float performed |
|
-take 2 to 3 grams of feces (1 teaspoon)
-mix in tube with zinc sulfate
-place a coverslip on top
-let sit for 10-15 minutes |
| |
|
how is a centrifuge fecal float performed |
|
-take 2 to 3 grams (1 teaspoon)
-mix in tube with zinc sulfate
-place a coverslip on top
-centrifuge for 5 minutes @ 1000-1500rpm
-let stand 10 minutes |
| |
|
what patients do we perform a direct fecal on |
|
-on puppies and kittens
-patients with diarrhea |
| |
|
what types of patient's would you perform a fecal sedimentation on |
|
on an icteric cat (to check for liver flukes) |
| |
|
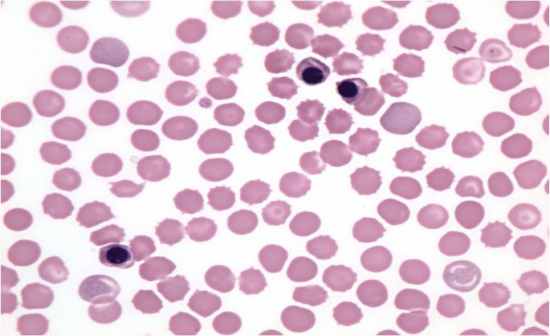
|
howell jolly bodies |
| |
|
|
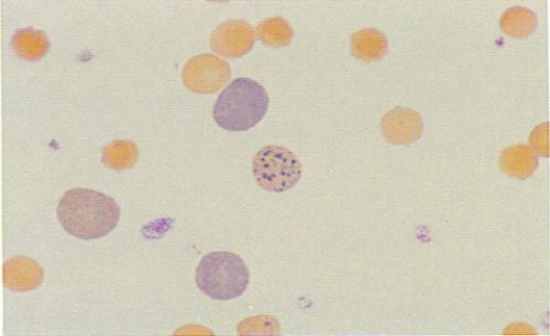
heinz bodies |
| |
|
|
heinz bodies |
| |
|
|
basophillic stippling |
| |
|
|
basophillic stippling |
| |
|
|
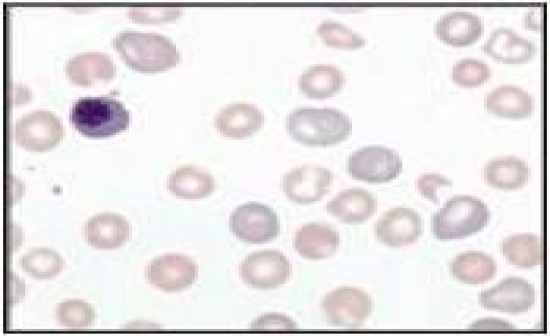
NRBC / metarubricyte |
| |
|
|
NRBC / metarubricyte |
| |
|
|
cytauxzoon felis |
| |
|
|
mycoplasma haemocanis |
| |
|
|
mycoplasma haemofelis |
| |
|
|
babesia |
| |
|
|
babesia |
| |
|
how can you tell if the mycoplasma is canis or felis |
|
-feline: has small dots on the border of RBC
-canine: has rods on border of RBC |
| |
|
how can you tell the difference between a lymphocyte and a NRBC |
|
-lymphocyte: sky blue cytoplasm less than in amount than nrbc
-nrbc: cytoplasm will be similar in color to surrounding RBC's and the nucleus will be darker with looser chromatin structure |
| |
|
|
mycoplasma |
| |
|
|
PAHN |
| |
|
|
humidity |
| |
|
|
reticulocytes |
| |
|
|
nrbc |
| |
|
|
polychromasia |
| |
|
which breed of dog will typically have degranulated eosinophils |
|
greyhounds |
| |
|
how is a direct fecal smear performed |
|
-place a drop of saline on a slide
-add a very small amount of fresh stool
-place a coverslip over it
-read immediatly and check for motility
-should be 50% / 50% of rods and cocci
|
| |
|
what are you looking for on a direct fecal smear |
|
-motility
-clostridium
-spirochetes
-giardia |
| |

|
|
clostridium |
| |
|
how is a fecal cytology performed |
|
-very thin amount of feces from rectal scraping
-apply with cotton swab on slide
-air dry and diff quick |
| |
|
how is a fecal sedimentation performed |
|
-mix 2 grams of feces and soapy water
-strain through gauze
-pour into centrifuge tube and centrifige for 3 to 5 minutes
-pour off liquid (like urine sediment)
-pipette small amountof sediment onto a slide and add coverslip |
| |
|
what type of test is the McMasters Technique |
|
-used in zoos
-parasite load
-mainly used on hoofstock
-it is a QUANTITATIVE TEST
-similar to unopette |
| |
|
|
McMasters Technique |
| |

|
|
Baermann Technique |
| |

|
|
baermann apparatus |
| |
|
why do we do baermann techniques |
|
-it is a sedimentation technique
-used for large animals |
| |
|
what parasite causes ocular larva mirgrans |
|
roundworm (toxocara cati/ canis) |
| |
|
what parasite causes cutaneous larval mirgrans |
|
hookworms (ancylostoma caninum) |
| |

|
|
roundworm (toxocara cati/canis) |
| |
|
|
roundworm (toxocara cati/canis) |
| |
|
|
hookworm (ancylostoma caninum) |
| |
|
|
hookworm (ancylostoma caninum) |
| |

|
|
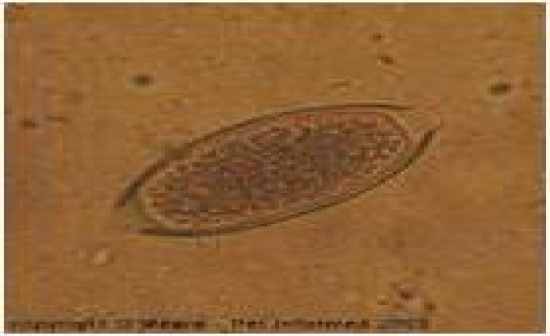
whipworm (trichuris vulpis) |
| |
|
|
whipworm (trichuris vulpis) |
| |
|
|
tapeworm (dipylidium caninum) |
| |
|
|
tapeworm (dipylidium caninum) |
| |
|
|
tapeworm (dipylidium caninum) |
| |

|
|
coccidia (isospora canis) |
| |

|
|
coccidia (isospora canis) |
| |
|
|
giardia |
| |
|
|
giardia |
| |
|
|
giardia cyst |
| |
|
what part of the cell do dohle bodies appear |
|
in the cytoplasm |
| |
|
what part of the cell does degenerative neutrophil changes take place in |
|
in the nucleus |
| |
|
in what part of the cell does toxic neutrophil changes take place in |
|
in the cytoplasm |
| |
|
what is the scientific name for the liver fluke |
|
platynossum fastosumm |
| |
|
|
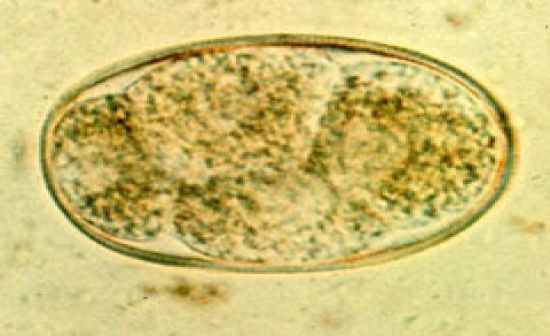
liver fluke (platynosomum fastosum) |
| |
|
what are the four signs of regeneration |
|
-polychromasia
-anisocytosis
-howell jolly bodies
-NRBC |
| |
|
what do you look for in a fecal direct and cytology |
|
bacteria, yeast
-must quantitate (+,++,+++) |
| |
|
what do you look for in a fecal float and sediment |
|
ova |
| |
|
what are the two protozoan intestinal parasites seen in feces |
|
-coccidia (isospora canis)
-giardia |
| |
|
what is the S.G of most floats |
|
1.200-1.250 g/ml |
| |
|
what is rhe S.G of most parasite ova |
|
1.100-1.200 g/ml |
| |
|
what does melana mean |
|
the passing of dark, black, tarry feces |
| |
|
if a patient has frank blood in their stool, where are they bleeding from? what is it called? |
|
-it is when fresh, bright blood is passing in the stool
-bleeding from the lower GI (probably the colon)
-it is called "hematochezia" |
| |
|
if a patient has dark, black, tarry blood in their stool, where are they bleeding from? what is it called? |
|
-bleeding from the upper GI
-called "melana" |
| |
|
what might a cat look like if they have mycoplasma |
|
-they are anemic
-they are weak, pale, and sometimes icteric due to the loss of blood |
| |
|
|
ehrlichia morulae |
| |
|
what is the best test to find whipworms |
|
centrifuge floatation |
| |
|
what is the best test to find roundworm |
|
floatation |
| |
|
what are some tests that are used to find liver flukes |
|
direct and sedimentation |
| |
|
what does it mean if you see retics |
|
it indicates regeneration |
| |
