|
What is the difference between stress and a stressor? |
|
Stressor: The cause - An agent or factor that triggers the stress response, usually threatens to overwhelm homeostasis
Stress: The effect, a generalized nonspecific response of the body to a stressor |
| |
|
Describe the generalized stress response (3 points) |
|
- Activation of the sympathetic nervous system
- Release of adrenocorticotropic hormone (ACTH) from anterior pituitary (hypothalamic-pituitary-adrenal-axis, HPA)
- The release of ACTH is controlled by corticotropin releasing hormone (CRH), released from nerves originating from the paraventricular nucleus (PVN) in hypothalamus. |
| |
|
Draw a flow diagram of the bodys respose to stress. |
|
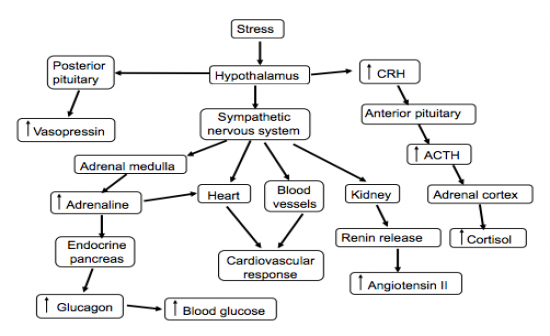
See image (needs more detail). |
| |
|
Draw a flow diagram outlining the bodily reaction to increased cortisol release from the adrenal cortex. |
|
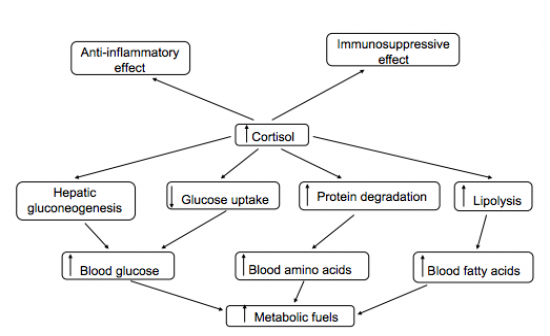
See Image. |
| |
|
What is the bodys physiological response to sychological stress? |
|
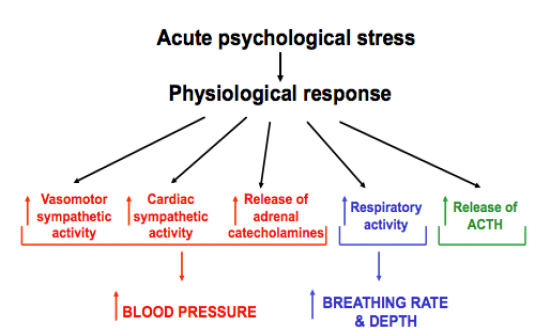
See Image. Response is very similar to cardiovasculatory responses which are evoked during exercise.
Example of physiological response to psychological stress: Cardiovascular events in Munich during the World Cup (2006). |
| |
|
How can environmental stress effect BP? Give example? |
|
Study comparing lay women to nuns, showed lay women to have significantly higher blood pressure over a long period of time, blood pressure significantly increased with age. As for Nuns, blood pressure remained relatively stable. This study showed that environmental stress could have long term effects on BP. |
| |
|
Which main brain region generates the cardiovascular response to stress? |
|
The Anterior cingulate cortex (ACC). Studies showed that lesions of the ACC prevent the cardiovascular responses to mental stress. |
| |
Which brain regions generate responses to stress?
Specifically what are the main responses of:
- PVN
- DMH
- RP
- VRG
- SNA |
|
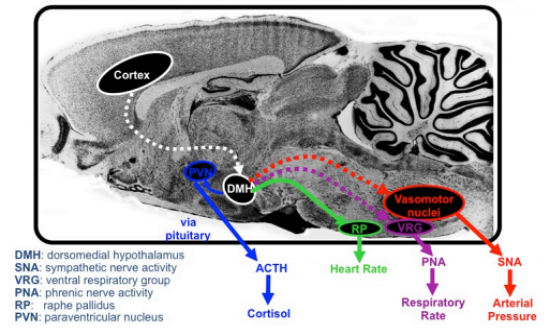
See Image.
- VRG: affects major nerve (phrenic nerve) that controls the diaphragm hence controls the rate and depth of breathing.
- RP: controls HR
- PVN: regulates release of ACTH --> Cortisol, controlling sympathetic outflow. |
| |
|
What evidence showed that the DMH is one of the key nuclei in triggering the physiological response to a stressor? |
|
Study in mice, showed that inhibition of the DMH (using muscimol and agonist of GABA receptors) blocked the CV response to air jet stress, for both BP and HR. |
| |
Draw a:
i) Sympathetic autonomic neuron
ii) Parasympathetic autonomic neuron |
|
Check book: Sympathetic has short pre and long post
Parasympathetic has long pre and short post - allowing the parasympathetic ganglia to be very close to the target organ. |
| |
|
What factors account for the marked difference in cardiovascular responses to standing up and passive tilt? |
|
In both cases change to upright position causes a shift of 500-1000mL of blood from thorax to lower part of th body (from above to below the hydrostatic indifference point)
The marked difference is due to the leg and abdominal muscle contractions involved in standing up which contribute to the muscle pump mechanically aiding in increasing blood flow back to the heart. This mechanism is not involved in passive tilt. |
| |
|
Outline the physiological response to passive tilt. |
|
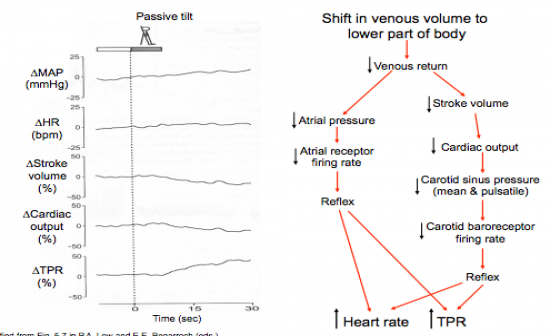
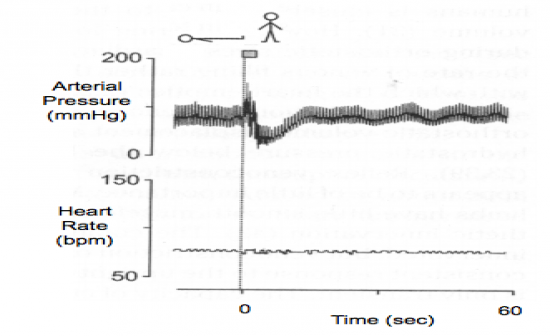
See image:
- Baroreflex and atrial receptors cause an overall increase in HR and TPR. |
| |
|
Outline the physiolohgical response to standing up. |
|
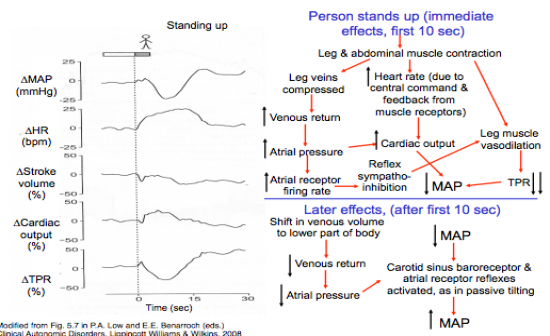
See image:
Immediately (first 10 seconds): Leg and abdominal muscle contractio - muscle pump
Later effects (after 10 seconds): Baroreceptor and atrial receptor reflexes as in passive tilting. |
| |
|
What is microneurography? |
|
Meaduring activity of a single nerve fibre to measure the overall level of sympathetic nerve activity. |
| |
|
Describe the response in HR and MAP after standing, if the carotid sinus was denervated? |
|
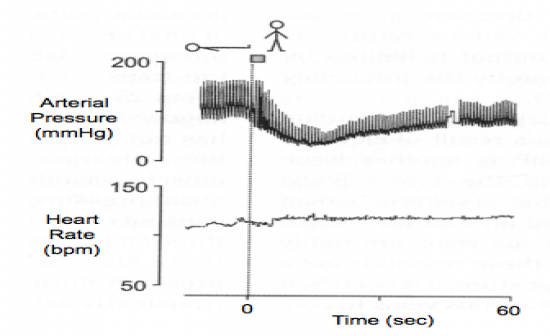
Compensatory response would still be present, but impaired. |
| |
|
Describe the response in HR and MAP after standing if there was cardiac denervation? |
|
The arterial pressure would be rapidly restored but not change in HR. Hence reflex vasomotor effects are sufficient for full compensation. |
| |
|
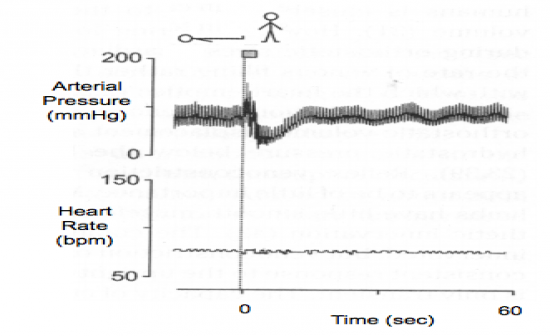
Describe the effect orthostatic hypothension (impairment due to vasomotor and cardiac autonomic control) would have on MAP and HR after standing? |
|
An initial rise in arterial pressure (prehaps due to transient increase in venous return), but no compensation for subsequent decrease in venous return and cardiac output. |
| |
|
Describe the effect of orthostatic hypothension (impairment of vasomotor control although cardiac control is normal) |
|

The cardiac reflex effects are not sufficient to compensate for the decrease in venous return. |
| |
|
Define syncope, and its cause? |
|
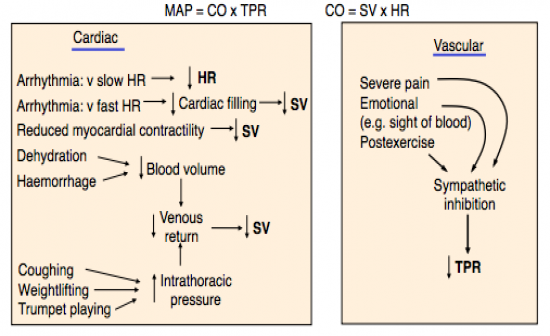
Syncope (fainting): Transient loss of consciousness
Cause: Inadequate cerebral blood flow, due to decrease in arterial pressure below autoregulatory threshold.
See image for other specific causes. |
| |
|
What is the normal range of body temperature? |
|
36-38 degrees.
Varies with circadian rhythms. Lower in the morning and higher in the afternoon. |
| |
|
What prevents the body from overheating? |
|
During exercise muscle temperature rises, and heat now flows from the muscle to the blood. Muscle blood flow is increased so that heat from the core can be transferred to the skin primarily by convection (increased blood flow to the skin).
Other heat loss will be lost through the evaporation of water from the respiratory tract, and increased ventilation rate.
Other heat is lost through evaporation of sweat. |
| |
|
List and describe the 4 main methods of heat loss. |
|
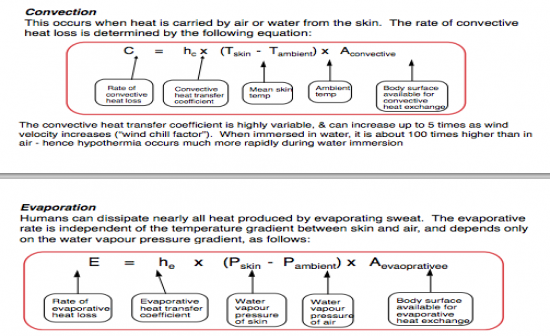
1. Radiation: heat lost by skin
2. Condiction: Skin contact with surface
3. Convection: heat carried out by air and water from skin eg breeze
4. Evaporation: Sweat.
See image for formulae. |
| |
|
What physiological factors limit the effectiveness of evaporative heat loss? |
|
- Dehydration (reduces sweat)
- Any factor reducing increased cardiac output (eg heart failure etc)
- A reduced ability to redistribute cardiac output to the skin |
| |
|
Draw diagram showing the firing rates for warmth and cold receptors as a function of skin temperature. |
|
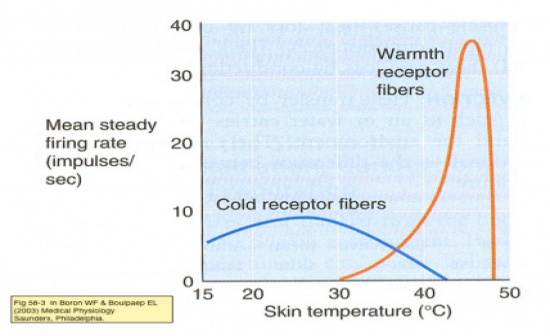
See Image. |
| |
|
Which two centres in the hypothalamus control heat conservation and heat loss? |
|
Heat conservation = Posterior Hypothalamus
Heat loss = Preoptic area |
| |
|
Draw a flow diagram for the efferent mechanism of heat gain. |
|
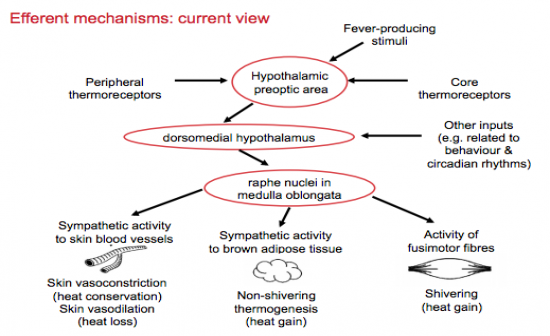
See Image. |
| |
|
Where are the sites of brown adipose tissue in adult humans and when are they activated? |
|
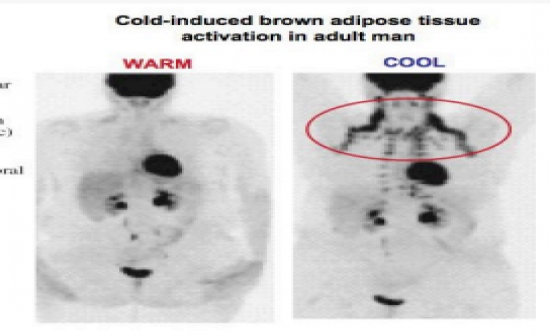
Brown adipose tissue in adult humans is found on the neck, shoulders and along the spine. It is activated during cool conditions. |
| |
|
Draw the thermoregulation output pathway. |
|
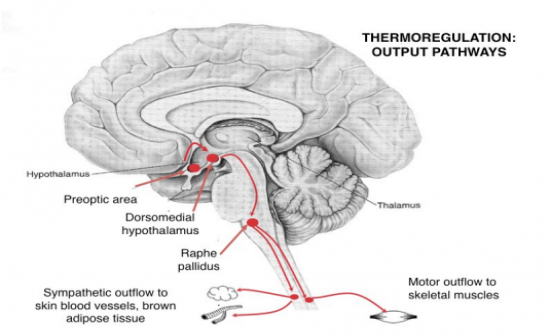
Preoptic Area --> DMH--> Raphe Pallidus--> Sympathetic outflow to skin blood vessels and brown adipose tissue. Motor outflow to skeletal muscle. |
| |
|
Draw the thermoregulation input pathways. |
|
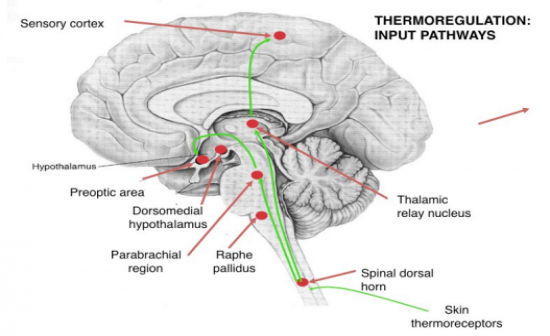
Skin thermoreceptors-->Spinal dorsal horn--> Raphe palidus --> DMH--> Preoptic area.
OR from Spinal dorsal horn--> Thalamic relay nucleus --> Sensory cortex |
| |
What are the main functions of:
- RVLM
- Raphe palidus
- VRG
- Vagal preganglionic neurons |
|
- RVLM: Regulating sympathetic outflow to heart, blood vessels and adrenal medulla
- Raphe pallidu neurons: Regulate sympathetic outflow to skin, blood vessels and brown adipos tissue, and motor output controlling shivering - VERY important to thermoregulation - dMRI studies confirm this - this area is activated in cool condition.
VRG: Control respiratory activity
Vagal preganglionic neurons: regulate heart rate |
| |
|
How does a virus lead to raised body temperature (fever) and why? |
|
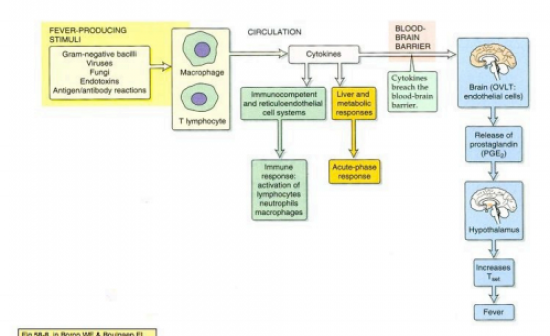
Pathway see image: Fever is developed to kill bacteria as bacteria are more suseptible to death at higher temperatures. |
| |
|
Why is exercise performance impaired under hot conditions? |
|
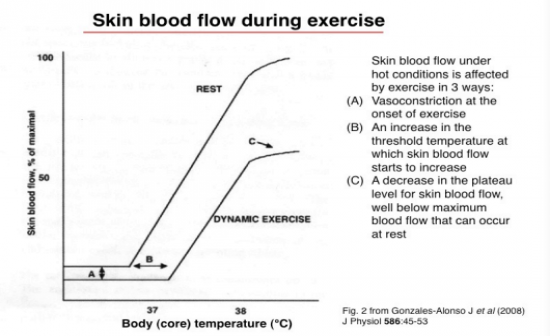
- Under hot conditions head causes dehydration which reduces the blood volume and hence venous return and cardiac output.
- Also compramised blood flow to skin hence less heat can be removed as the blood flow is redirected to the skeletal muscle. |
| |
Effects of progressive dehydration and hyperthermia in prolonged high level exercise include:
1. Gradual decrease inc ardiac output and stroke volume
2. Gradual increase in adrenaline, noradrenaline and heart rate
3. Sharp increase in leg lactate after 90min
Why? |
|
1. CO and SV decrease as dehydration is progressively setting in which will result i a decrease in blood volume which will result in decreased CO and SV. Hence hydration is absolutely essential.
2. Adrenaline and noradrenaline are increased due to a gradual increase in sympathetic activity which explains the gradual rise in HR.
3. Sharp increase in lactate after 90min indicates the point at which blood glucose stores are depleted and anaerobic metabolism becomes more important. |
| |
|
How does the renin-angiotensin-aldosterone system increase BP and BV? |
|
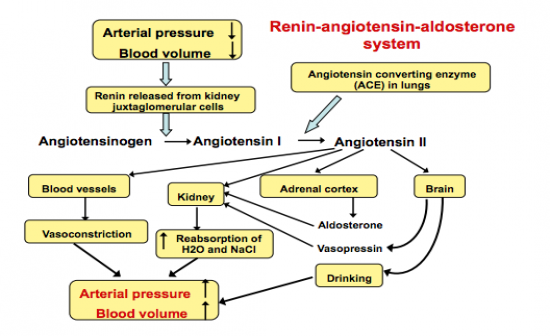
See image.
AngII acts on kidneys in 3 ways. 1 direct way and 2 indirect. |
| |
|
If angiotensin II does not cross the blood brain barrier, then how does it act on the brain? |
|
It acts on recetors on neurons on the brain - circumventricular organs. Ang type I receptors (AT1) --> neurons project.
In patients with raised levels of sympathetic activity, blockade of AT1 receptors can reduce sympathetic activity. |
| |
|
Draw the renal dunction curve and describe how the sympathetic nerves can affect this. |
|
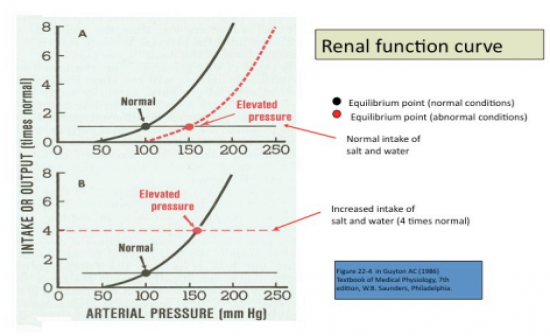
See Image.
Graph shows the relationship between arterial pressure and renal output of salt and water. The pressure can only increase if:
i) Renal function curve moves to the right
ii) The intake of salt and water is increased.
Sympathetic nerves can only affect long-term level of blood pressure by affecting the renal function curve either:
i) directly via an action on renal vascular resistance or
ii) indirectly via release of renin from the kdney or via release of catecholamine |
| |
|
What is noradrenaline spillover and what is its relationship with renal sympathetic nerve activity? |
|
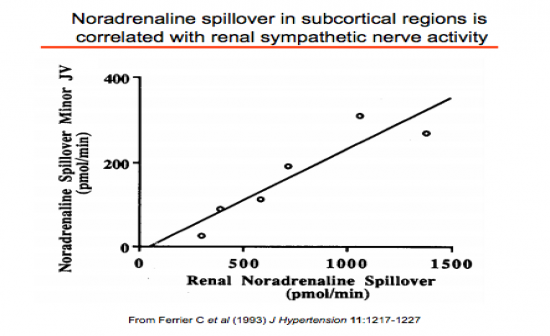
Noradrenaline spillover is when release is greater than reuptake and can be used to measure the degree of activation of noradrenergic nerves. It can be linked with increased heart failure and hyptertension.
|
| |
|
How does the DMH control the generation of circadian rhythms? |
|
The DMH regulates the set-point of the baroreceptor reflex. Thus chronic activation of the DMH by stress-associated inputs could reset the baroreflex to higher pressure levels |
| |
|
How can resetting the baroreflex-SNA curve lower blood pressure levels? |
|
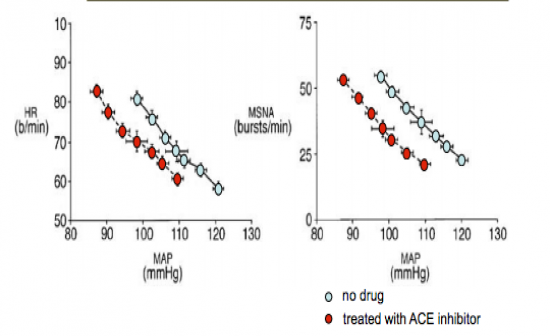
In humans with hypertension, blockade of renin-angiotensin system re-sets the baroreflex-SNA curve to lower blood pressure levels.
Also in humans with heart failure, blockade of renin-angiotensin system lowers SNA.
|
| |
|
How does leptin effect blood pressure and body weight? |
|
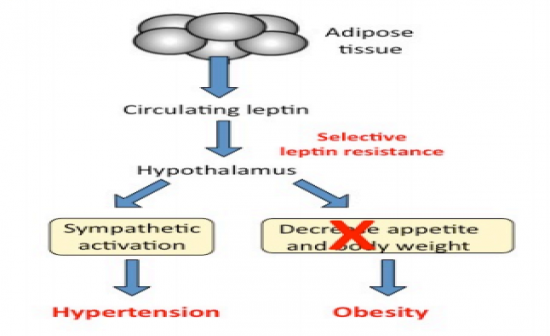
Leptin, released from adipose tissue and circulates in blood, acts on hypothalamus and has extreme effects on appetite and weight. |
| |
|
Draw interactive flow chart of main brain centres contributing to blood pressure. |
|
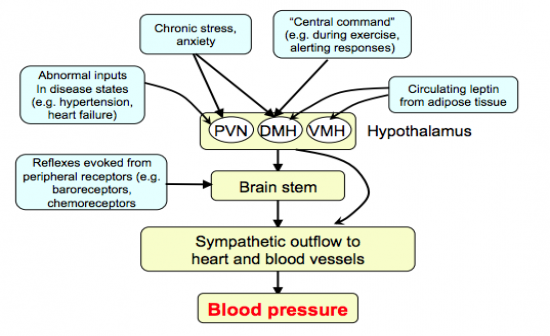
See image. |
| |
|
What is Noradrenaline spillover an indicator of? |
|
Indicator of sympathetic activity |
| |
|
Sympathetic nerve activity in humans is.. |
|

Greatly increased in severe heart failure.
|
| |
|
How do the AT1 receptors level change in the PVN and medulla in people with heart failure? |
|
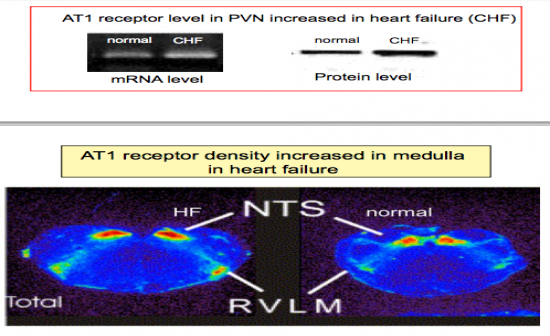
Increase. |
| |
|
How is the cardiac sympathoexcitatory reflex effected in heart failure? |
|
Enhanced. This enhanced response is normalized by injection of an AT1 receptor blockade into the NTS. |
| |
|
How are nNOS levels in brain effected in heart failure? |
|
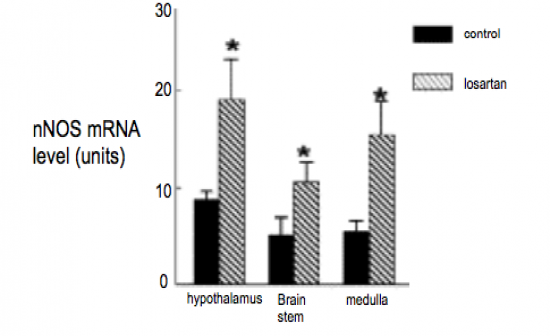
Levels are reduced in the brain stem and hypothalamus. These reduced levels can be restored by systemic administration of AT1 receptor antagonist (losartan) |
| |
|
What is Patel's hypothesis? |
|
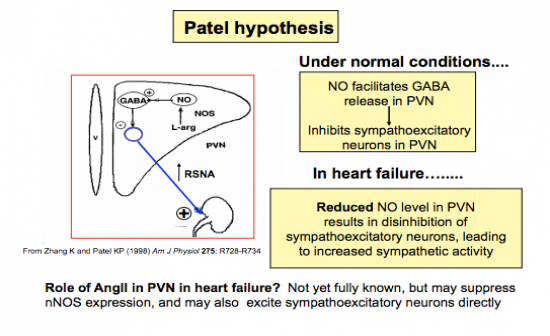
Patel's hypothesis is that under normal conditions NO facilitates GABA release in PVN, which inhbits sympathoexcitatory neurons in the PVN.
However in heart failure, reduced NO levels in PVN results in disinhibition of sympathoexcitatory neurons, leading to increased sympathetic activity. |
| |
|
Draw intergrative pathways of how increased sympathetic activity is sustained. |
|
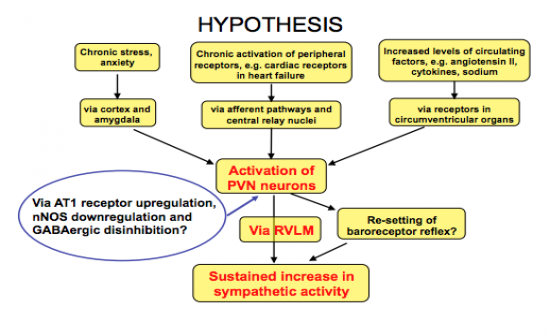
See image. |
| |
