Related Flashcards
Cards In This Set
| Front | Back |
|
What are the functions of the stomach?
|
· Storage – 80% of food is stored in the proximal stomach (the gut works slowly)
· Mechanical disruption – grinds/churns food
· Digestion – acid, pepsin
· Bactericidal barrier
· Exocrine, paracrine, & endocrine secretions
|
|
ARS: Which of the following is the only essential product of the stomach?
A) Acid
B) Pepsinogen
C) Mucus
D) Intrinsic Factor
|
Answer: Intrinsic Factor (For vitamin B12)
|
|
Where are parietal cells located and how do they secrete acid?
|
In gastric pits.
Fuse tubovesicles together to form intercellular canaliculi in active state to increase surace area for acid secretion (takes about 10 min to go from resting to active stage - major cell remodeling)
|
|
What is the difference in gastric juice composition with a slow rate vs. a fast rate?
|
Low flow rates: High Na+, high Cl- (at night, for example) – secretion comes from surface epithelium cells
Max flow rates: almost entirely HCl (surface epithelium doesn’t stop secreting Na+, but the parietal cells are secreting so much HCl that it dilutes out the Na+)
At very high secretion rates, individuals may produce 6-40 ml/h of HCl at a conc. of 0.1-0.2 M. At these rates, gastric juice tends to become isotonic w/ plasma – aqueous component contains little or no HCO3 to buffer HCl so pH can be pushed to 0.8 –1
|
|
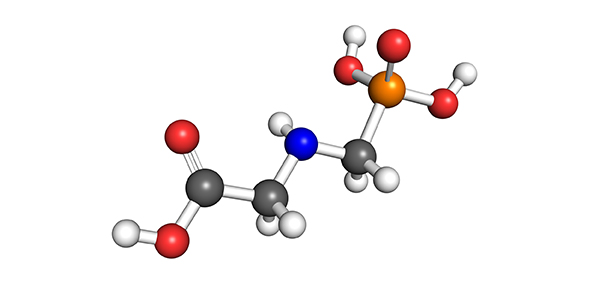
What is the mechanism of acid secretion from the parietal cells?
|
1:1 exchange of H & K (H/K ATPase – this is the pump that’s inhibited by drugs like Omeprazole & PPIs) – active transporter; move H against a gradient so need ATP. For it to work, need the following:
- Must have a K channel to let K out of cell b/c you are exchanging a K in the ATPase (K cycles futilely b/t the pump & channel)
- H can’t exist by itself, needs Chloride for electroneutrality: Cl channel – Cl- leaves cell down its gradient in lumen of stomach. How can cell do this? Cell stuffed full of carbonic anhydrase which gives you bicarbonate from CO2 & water). Bicarbonate gets thrown out and Cl- comes in (exchange bicarb for Cl- on basolateral membrane = “alkaline tide” right where the pump is working hard)
- Always have a Na/K pump in the basolateral membrane & a K leak channel
- Also, have a Na/H exchanger to “mop up” any leftover H+ that’s inside the cell & get it out of the cell
|
|
Which hormones that cause acid secretion use the Gq protein and what are their receptors?
|
Gastrin (CCK-B)
ACh (M3 muscarinic receptor)
|
|
Which hormones that cause acid secretion use the Gs protein and what are their receptors?
|
Histamine (H2)
|
|
Pathway for acid secretion:
|
All three hormones (gastrin, ACh, histamine) work to initiate remodeling through the canaliculi (and release of H through getting the H/K ATPase up to the membrane)
- Gastrin & ACh both coupled to PLC --> IP3 --> increase intracellular calcium (released from ER)
- Histamine - released from from ECL (enterochromaffin-like) cells & binds to H2 receptor (Ranitadine blocks these) à activates Gs à activates AC (?) à increase in cAMP à increase in PKA phosphorylation
|
|
What hormones inhibit acid secretion through Gi?
|
Somatostatin
Prostaglandins
|
|
What is the effect of eating on acid secretion?
|
Food is like a "buffer".
Eating increases volume in stomach (distention) - also proton conc. drops & pH increases --> triggers acid secretion
At 1 hr post-eating, stomach begins to empy & amount of buffers decreases. Proton secretion continues to rise.
3 hrs. post-eating, stomach is really empyting; acid secretion statrs to decrease
|
|
What is the negative feedback mechanism for acid secretion?
|
Process:
Input from Vagus à ACh à acts on postganglionic neuronàcauses release of GRP (gastrin-releasing peptide) à G cell releases gastrin (hormone) that goes into the blood & finds its targets. Small peptides & AAs can also trigger G-cells
Negative Feeback:
At the same time (all happening in the antrum) – vagus causes an inhibitory neuron to secrete ACh to keep the somatostatin-secreting cell quiet. When pH gets below 3 the SS cell is triggered to “go next-door” and stop G cell production of gastrin (PARACRINE RELATIONSHIP). D cells work in close contact w/ ECL cells to release somatostatin when pH gets too low and in response to gastrin
|
|
Describe the process of inhibition of gastric secretion:
|
· Oxyntic gland (aka gastric glands) are stimulated by pH<3 to release somatostatin
· Antrum stimulated by pH<3 to release somatostatin
· Duodenum stimulated by acid & hyperosmotic solutions to release secretin
· Duodenum & Jejunum stimulated by fatty acids to release GIP
|
|
What does mucus do?
|
Protects against auto-digestion
|
|
How is mucus divided up in the stomach?
|
Loosely adherent layer (lower HCO3 conc. than the firmly adherent layer) & firmly adherent layer
|
|
How does mucus work and what produces it?
|
The glycoproteins are important in trapping bicarbonate to prevent back-diffusing acid.
Surface epithelial cells (visible) & mucous neck cells (soluble) secrete mucins & HCO3 (bicarb) that form a mucus layer coating the stomach – in response to vagal efferent nerves.
This alkaline mucus layer acts as a protective barrier (keeps pH of mucosa at 7) to gastric acid & pepsin.
|