Related Flashcards
Cards In This Set
| Front | Back |
|
What are 3 generic structural features of cephalosporins? (How does each compare to penicillin?)
|
1. B-lactam ring (same as penicillin)2. Six-membered ring containing sulfur fused to B-lactam ring (vs. penicillin's 5-membered thioazole ring)3. Two variable R-groups (penicillins have one)
|
|
Are cephalosporins bactericidal or bacteriostatic?
|
Bactericidal.
|
|
How do cephalosporins work?
|
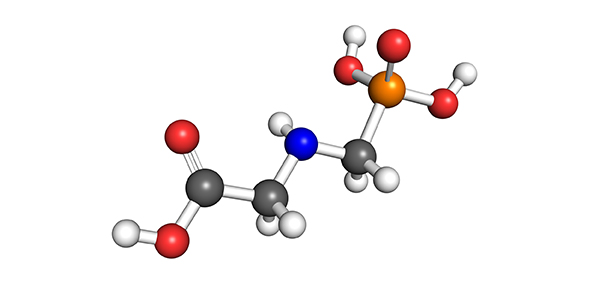
Like all B-lactams, they inhibit transpeptidase, a PBP that cross-links peptidoglycans in the cell wall of Gram+ bacteria. Specifically, they mimic the structure of dimerized alanine, which transpeptidase links to a lysine of a neighboring peptidoglycan. Once the bacterial cell wall is compromised, an autolytic program is activates and the bacterium lyses.
Note: the penultimate alanine is linked to the neighboring lysine; the last alanine falls off. |
|
What are three mechanisms of resistance to cephalosporins? Which are most clinically significant?
|
1. B-lactamases cleave the B-lactam ring (MOST clinically important)2. Mutant PBPs have lowered affinity for cephalosporin (also important)3. Efflux (pumping out) of drug from target cell (not so important)
|
|
How are cephalosporins administered?
|
1st, 2nd, and 3rd generation: oral, IM, and IV4th generation: IV only.
|
|
Cefoxtaxime has a shorter half-life and lower max concentration in the blood than ceftraixone, but a higher max concentration in the CSF (both are 3rd gen). How is the possible?
|
Half-life in blood is not the same as half-life in CSF; ceftriaxone has a longer half-life in CSF than cefotaxime.
|
|
Why wouldn't you use 1st or 2nd generation cephalosporins to treat meningitis?
|
Poor distribution to CSF
|
|
How are cephalosporins metabolized/excreted?
|
Minimal metabolism. Cephalosporins are mostly excreted renally. Some are eliminated hepatically (preferable for patients with renal insufficiency).
|
|
What are advantages of 1st generation cephalosporins?
|
Good activity against Gram+ bacteria (only moderate against Gram-).
|
|
What are clinical uses of 1st generation cephalosporins?
|
Uncomplicated streptococcal and staphylococcal infection.
|
|
What are advantages of 2nd generation cephalosporins?
|
Increased activity against Gram- organisms relative to 1st generation.
|
|
What are clinical uses of 2nd generation cephalosporins?
|
Gram+ organisms (not as good as 1st gen)Some Gram- organisms: E. Coli, Klebsiella, Proteus
|
|
What are advantages of 3rd generation cephalosporins? (Ceftriaxone)
|
1. Excellent activity against Gram- organisms. (Not so good for Gram+.)2. More resistant to B-lactamases (vs. 1st and 2nd gen)Note: B-lactamase is still the most clinically important mechanism of resistance against 3rd generation cephalosporins)3. Therapeutic distribution to CSF (vs. 1st and 2nd gen)
|
|
What are clinical uses of 3rd generation cephalosporins?
|
S. pneumoniae (Gram+, but B-lactamase makes it resistant to 1st/2nd generation)NisseriaN. meningitides (bacterial meningitis)P. aeruginosa
|
|
What are advantages of 4th generation cephalosporins?(Cefapime)
|
1. Broad spectrum: Good activity against both Gram+ and Gram-2. More resistant to B-lactamases (vs. 1st and 2nd gen)Note: B-lactamase is still the most clinically important mechanism of resistance against 3rd generation cephalosporins)3. Improved penetration in Gram- bacteria due to positive charge
|