|
Dental Caries Definition |
|
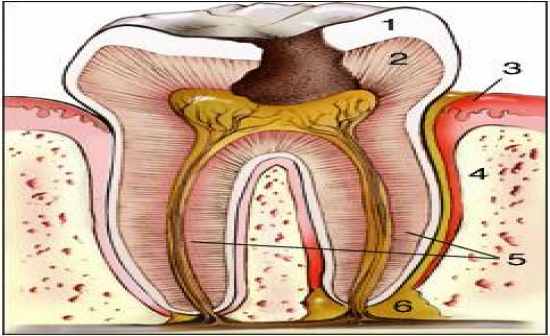
- this is a unique form of infection in that specific strains of bacteria elaborate acidic and proteolytic products that demineralize the enamel surface and digest the organic matrix
- they will progress through the dentin to the pulp, where it can penetrate further to infect the surrounding soft tissues resulting in pain and destruction
- may spread to bone marrow spaces and soft tissues of the face and neck |
| |
|
Dental Caries Correlates |
|
- prevalence and severity differ among different cultures and countries
- closely correlated with consumption of sugar (refined CHO, dental care and OH, as well as Fluoridation of water |
| |
|
Dental Carries Susceptibility |
|
- susceptibility to caries differs among different age groups and individual teeth
- young patients with high sucrose diets and poor OH are most prone to the pit and fissure caries (2nd molars followed by 2nd premolars) - highest susceptibility
- if the oral environment is extremely cariogenic then the smooth surfaces of molars and premolars will be affected (interproximal followed by buccal and lingual) |
| |
|
Types of Dental Caries |
|
- Pit and Fissure
- Smooth Surface
- Cemental
- Recurrent |
| |
|
Pit and Fissure Caries |
|

- these are the most common type of caries which can develop at an early age
- these will occur on the occlusal and buccal surfaces of the primary and permanent dentition
- these are also the most destructive carries |
| |
|
Smooth Surface Caries |
|

- these are less common located on the interproximal areas and occasionally on the cervical of buccal and lingual surfaces
- common in caries in infants who are sleeping with juice or milk in their bottle or milk
- also common in patients who undergo radiation therapy or have dry mouth |
| |
|
Cemental Caries |
|

- these caries are usually found in older patients in teeth with gingival recession
- these will have a rapid progression to the pulp
|
| |
|
Recurrent Caries |
|

- caries which develop around an existing restoration
- these situations predispose a tooth to the accumulation of bacteria and food in an environment protected from the usual hygiene procedure
- different rate of progression depends on the patient diet and hygiene habits |
| |
|
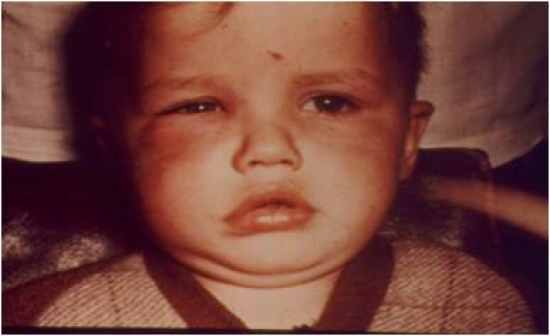
Acute (Rampant) Caries |
|

- these are in young patients with large pulpal chambers and wide, short dentinal tubules
- patients with a high sugar diet and poor OH
- caries progress rapidly and penetrate into the pulp |
| |
|
Chronic Caries |
|
- these are seen in older patients with a smaller pulp
- pulps with deposits of denser and less tubular dentin on pulpal walls called secondary dentin (also tertiary present)
- pain is not as severe as in acute caries |
| |
|
Pulpitis |
|
- an inflammation of the pulpal tissue that may be acute or chronic, with or without symptom, and reversible or irreversible
- patient will develop symptoms from an inflammation of the pulp |
| |
|
Reversible Pulpitis |
|
- this is a case in which the pulp is capable of a full recovery if the irritating factors subside or are removed
- remedy is protecting the pulp from further injury
- symptoms - pain is sharp and last less than 20 sec - elicited pain, not spontaneous; unaffected by body position and is easily localized
- histologically characterized by increased vascularity of the tissues |
| |
|
Irreversible Pulpitis |
|
- the pulp will most likely not recover, regardless of the attempts to treat it
- we have common diagnostic techniques to determine irreversible from reversible pulpitis (history, thermal, electric, percussion, radiographic, visual, palpation) |
| |
|
Acute Pulpitis |
|
- the patients are younger and the pulp chamber is closed
- the pain is spontaneous and affected by body position which is often difficult to localize
- this can be dull or sharp, but more intense and lasting more than 20 sec, and responds with higher voltages to the electrical stimulation or no response |
| |
|
Chronic Pulpitis |
|
- this is present in an older tooth which is caused by a low grade irritant
- smaller pulp chamber with a fibrotic pulp, pulp stones, or dystrophic calcification with sclerotic dentinal tubules
- dull and low intensity pain, or no pain at all |
| |
|
Pulp Polyp (Chronic Hyperplastic Pulpitis) |
|

- this is present in molars of children and is a result of rampant caries
- this is often an open pulpitis meaning that the pulpal tissue will proliferate and produce granulation tissue
- this is asymptomatic, results inepitheliual migration of tissue to surround the pulp |
| |
|
Periapical Lesion Definition |
|
- infection of the periodontal tissues around the apex depending on a variety of factors including the host, MO, environment, etc
- the nature and behavior of the lesion depends on the presense of open/closed pulpitis, virulence of MO,extent of sclerotic dentin and competency of the host system |
| |
|
Chronic Apical Periodontitis |
|
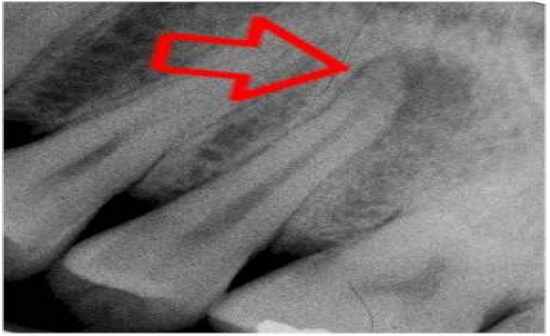
- this is the earliest radiographic evidence of extensionof the inflammatory process from the pulpal chamber into the adjacent periodontal membrane around the apical membrane
- this is a shadow of radiolucency = earliest sign of periodontitis
- a widened PDL, with faint evidence of vitality and a + reaction to percussion
- this is a transitory phase between the pulpitis and more distinct PA lesions |
| |
|
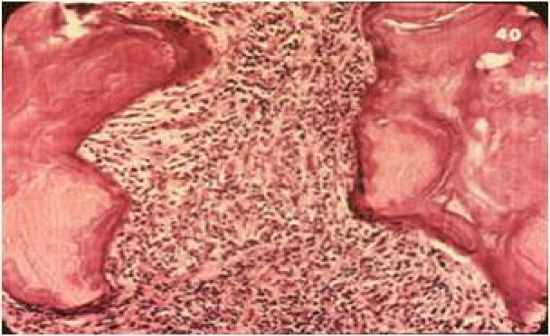
Periapical Granuloma |
|

- the is when the pulpitis processes into a periapical lesion
- most common lesion that occurs after pulpal necrosis (death of the pulpal tissue)
- no reaction to pulpal testing, but occlusal tests will cause pain due to PDL inflammation
- usually painless, may be associated with a draining exudate, if the open pulp chamber is blocked and drainage is inhibited, the PA lesion will transform into an apical abscess with pain
- the most common transformation is PA cyst |
| |
|
Periapical Abscess |
|
- the initial lesion that develops when circumstances are adverse
- apical granuloma which transitions due to a new MO activity or change in the immunologic system of the patient |
| |
|
Periapical Cyst |
|

- common development of long-standing, untreated periapical granuloma
- normal epithelium is scattered normally, but in some cases the lesion will be surrounded by epithelium thus becoming periapical cysts |
| |
|
Osteomyelitis (General Information) |
|
- this is an acute or chronic inflammatory process of the bone and its structures secondary to infection with pyogenic organisms
- due to a change in the virulence of the MO, this can extend the infection into the surrounding structures (IE - bone)
- this is an inflammatory process within the medullary (trabecular) bone that involves the marrow spaces |
| |
|
Acute Osteomyelitis |
|
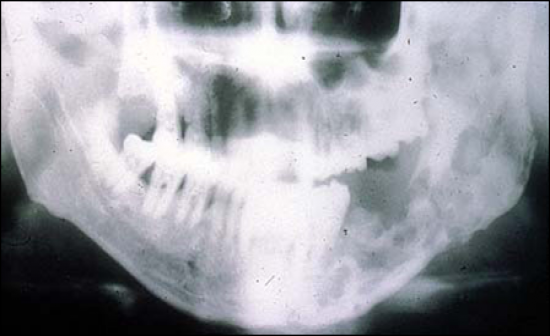
- a rapidly destructive inflammatory process within the bone that consists of granulation tissue, purulent exudate, and islands of non-vital bone also called sequestra |
| |
|
Chronic Osteomyelitis |
|
- this is a supparitive infection of the medulla of the bone which follows a chronic course with intermittent acute, or subacute exacerbations
- if you want to know if the bone is vital, you must look at the lacunar spaces and if they are empty this means that the bone is non-vital |
| |
|
Cellulitis |
|
- a painful swelling of the soft tissue of the mouth and face resulting from a diffuse spreading of purulent exudate along the fascial planes that separate muscle bundles
- very painful, associated with the area of infection around the region of the tooth in which the MO can break the immune barrier and spread along the facial planes - possible death |
| |
|
Ludwig Angina |
|
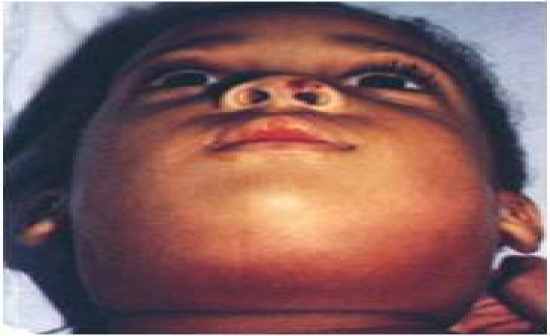
- Cellulitis involving fascial spaces between muscles and other structures of the posterior floor of the mouth that can comprise the airway
- involves the throat and the lfoor of the mouth which can cause swelling of the airway leading to the compromising of respiration |
| |
|
Sinus Tract |
|
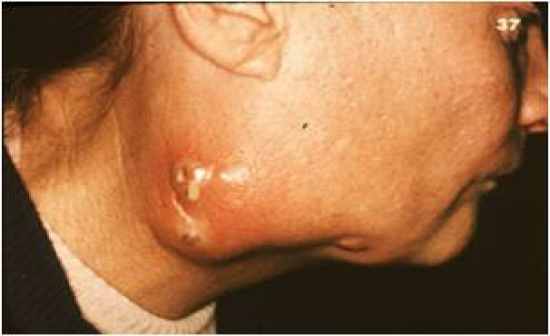
- a drainage patheay from a deep focus of acute infection through tissue and/or bone to an opening in the surface
- tube that connects the internal infection to the external environment (location depends on the location of the infected tooth)
- antibiotics can be given to help take care of the infection |
| |
|
Fistula |
|

- a drainage pathway or abnormal communitcaiton between two epithelium-lined surfaces due to destruction of the intervening tissue
- the fistula connects two cavities rather than just an infection and the exterior
- example - maxillary sinus and oral cavity |
| |
|
Parulis |
|

- a sessile nodule on the gingiva at a site where a drainage sinus tract reaches the surface
- a small soft tissue nodule you see in the gingiva where a sinus tract drains (sometimes associated with a raised lesion or a lump) |
| |
|
Condensing Focal Osteitis |
|

- when an irritating factor is of low enough intensity and when resistance of the patient is high that the reaction in the bone will produce bone in the PA region rather than resorption
- pathogenesis is essentially the same as chronic apical periodontitis
- can also be termed condensing osteitis or sclerosing osteitis
- treatment can lead to resolution or retention of the increased density in the bone |
| |
|
Garre Osteomyelitis |
|

- an unusual hyperplastic reaction of the periosteum to a chronic osteomyelitis of the posterior mandible that is unique to young patients
- young patients present with a radiopacity in the posterior mandible, plalpation results in a distinct reaction |
| |
|
Internal Resorption |
|

- resorption of the dentin from the pulp outwards
- the tooth often has a history of trauma or a pulp cap and discoloration may or may not be present
- pulp necrosis tests may indicate vitality or necrosis
- if treated early a RCT may be effective but too much dentin may be resorbed = weak enamel
- this is dentinoclastic activity leading to a well demarcated lesion with clear radiographic margins
- advanced cases may mimic localized periodontal problems (external resorption) |
| |
|
Dry Socket |
|

- this is an infection in the dental socket following the extraction of a tooth
- usually develops when a blood clot fails to form or if the blood clot becomes loose
- this occurs in about 5% of all tooth extractions
- the surface of the bone is exposed and leads to the symptoms, this is a form of osteitis |
| |
