Mineral Bioavailability
Decrease:
F_____
p______
Ox______
Mineral-______interactions
EX: calcium and iron
Enhance:
Vitamin-_______interactions
Ex: vitamin C and iron
Animal product sources _______________
|
|
Decrease: Fiber and phytate, Oxalates
Mineral-mineral interactions
EX: calcium and iron
Enhance:
Vitamin-mineral interactions
Ex: vitamin C and iron
Animal product sources generally best absorbed
|
| |
|
Minerals Most Likely to be Deficient in N. America |
|
Calcium
Iron
Zinc
|
| |
Major functions of minerals
F
E
A
S
BL |
|
Fluid balance
Energy Metabolism
Antioxidants
Structure (bones)
Blood components
|
| |
Fluid Balance: Four components?
S
C
P
P
What are Sources of each? Purpose of each?
|
|
Sodium
Table salt (NaCl):40% sodium, 60% chloride
Major (+) ion, extracellular fluid
Chloride
Table salt
Major (-) ion, extracellular fluid
Potassium
Fruits, vegetables, milk, grains, meats, dried beans
Major (+) ion, intracellular fluid
Phosphorous
Dairy and meats
20-30% from food additives
Soda contains phosphoric acid
Difficult to limit intake
|
| |
Food Manufactures Vs. Home Cooked:
How does sodium chloride get into our food? (%)
|
|
Where does it come from?
~15% added by individuals
~10% naturally occurring in foods
~ 75% added by food manufacturers |
| |
What minerals contribute to
Structure (Bones)? What are they found in?
|
|
Calcium
Makes up 40% of all the mineral present in the body
Has many functions in addition to bones
Magnesium
Plant products: legumes, seeds, nuts, whole grains, vegetables
Fluoride
Toothpaste, tea
Phosphorous |
| |
Calcium / Bone Mass Facts:
Peak mass age?
Loss begins age?
Major bone mass loss called? What is is? Who / what increased risk?
|
|
Peak bone mass: age 20-30
Bone loss begins: age 30-40
Significant loss at menopause
Osteoporosis
Poor bone structure
High risk: female, small frame, old age, low calcium intake, smoking, ED |
| |
Calcium Absorption: Enhancers / Inhibitors
Best source of calcium?
|
|
Absorption
Enhancers
Vitamin D, stomach acid
Inhibitors
Phytates, oxalates, tannins
Dairy is best source of Calcium
|
| |
Vegetarianism and calcium: challenges & tips
Challenge:
Difficult to ____ ____ without ____.
Some _____ sources are poorly absorbed
Tips:
Choose ________foods
Dairy ___________
T_____ (some types)
Some RTE ______, _______
Some green ________ |
|
Challenge:
Difficult to meet needs without dairy
Some plant sources are poorly absorbed
Tips:
Choose fortified foods
Dairy substitutes
Tofu (some types)
Some RTE cereals, snacks
Some green vegetables |
| |
Sulfur controls _____ base balance. Source?
Component of? |
|
Acid-base balance
Source: food proteins
Component of body protein |
| |
|
Two types of bones: |
|
Cortical or compact bone
Trabecular or spongy bone |
| |
|
Bone is composed of: |
|
a protein frame work, or matrix, hardened by deposits of minerals
|
| |
___________ is the most abundant protein
_____________ is the calcium-phosphorus crystal |
|
Collagen is the most abundant protein
Hydroxyapatite is the calcium-phosphorus crystal |
| |
Two types of iron in the diet? Each comes from where?
|
|
Heme iron: part of hemoglobin and myoglobin in animal products. Heme iron is absorbed more efficiently and less affected by other dietary factors
Nonheme iron: in plant foods and released from cooking utensils |
| |

Map basic chemical structure of heme iron.

 |
|
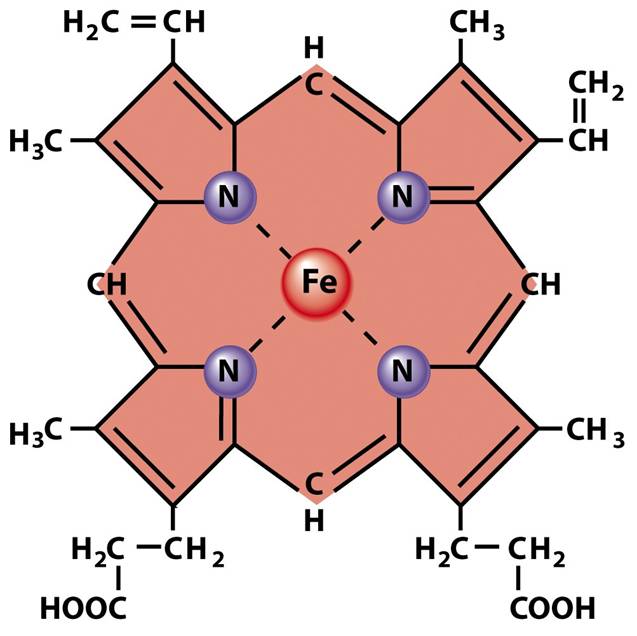
Fe chem structure
|
| |
|
Map path of HEME iron in digestive track |
|
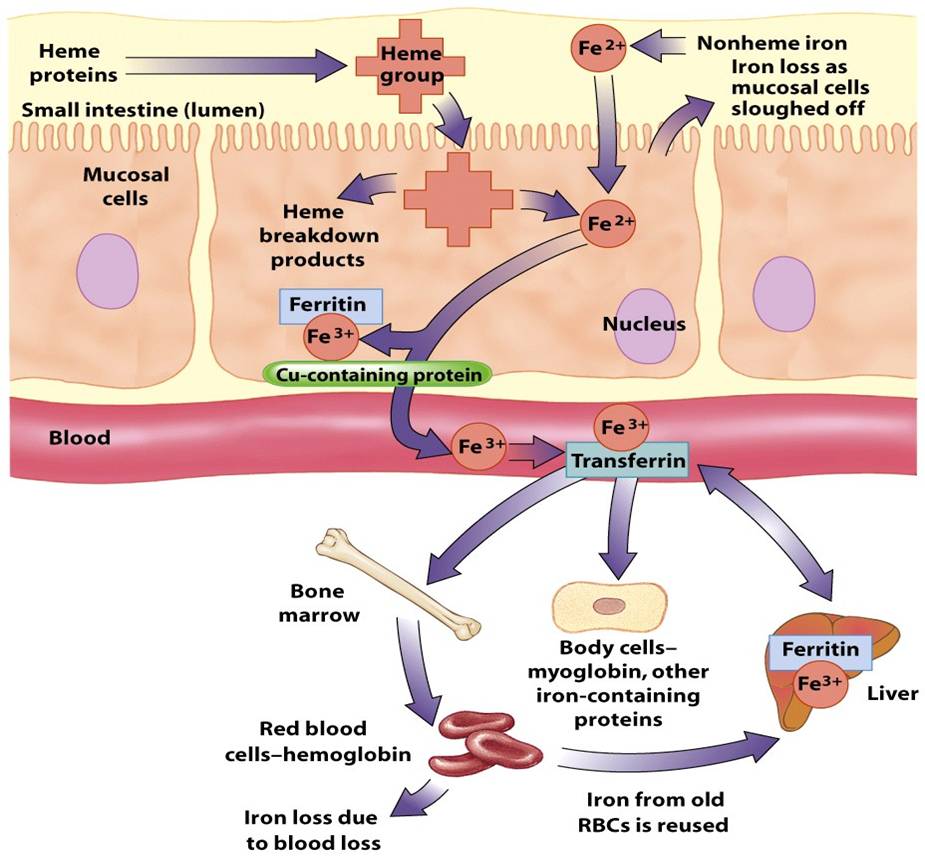
HEME path: a HEME group is absorbed in small intestine (lumen) at Mucosal wall. Breaks down into "breakdown products" and Fe2+.... Fe2+ joins Ferritin within the mucosal cell to become Fe3+. The Fe3+ joins with a CU-containing protein and moves into the blood stream. Fe3+ joins Transferrin in the blood stream. From blood stream, it goes bone marrow (red blood cells or hemoglogin), and body cells (myoglobin). Some Fe3+ goes to liver where it can pick up Ferritin because the liver stores iron from "old" red blood cells. Iron is also lost with blood loss.
|
| |
Absorption of nonheme iron is affected by many factors
|
|
Fiber, phytates, tannins, and oxalates bind to iron in the GI tract and reduce absorption
The presence of other minerals in a meal can decrease iron absorption (esp. calcium) |
| |
Map path of NON-HEME iron in digestive track
|
|
Non-heme iron enters the mucosal cell as Fe2+. Some is lost as mucosal cell is sloughed off. Some is retained and joins Ferritin to become Fe3+. Fe3+ joins with a CU-containing protein and enters the blood stream. In the blood stream, it joins with Transferrin and serves all the same processes as HEME iron (bone marrow - rbc, body cells, liver.
|
| |
Regulation of iron transportation
|
|
*Absorbed iron is bound to storage protein ferritin or picked up by the transport protein transferrin
*The transferrin-iron complex binds to transferrin receptors to deliver iron into cells
*The transferrin receptor gene is regulated based on amount of body storage iron |
| |
Iron stores and Iron losses:
|
|
Iron stores
In ferritin in the liver, spleen, and bone marrow
High levels of liver ferritin can be converted to hemosiderin
Iron losses
The body recycles iron
Blood loss and shedding of cells from intestine, skin, and urinary tract are major reasons iron is lost in healthy individuals
|
| |
Functions of iron
O
N
C
E |
|
*Delivery of OXYGENto cells via two oxygen-carrying proteins hemoglobin and myoglobin
*NEUROtransmitter synthesis in brain
*Normal immune function and drug metabolism*CO-factor for enzymes that protect cells from oxidative damage. A cofactor for many other enzymes
*ENERGY production
|
| |
Iron is in 3 locations in the body: The iron stores, the plasma and the red blood cells. In what order does iron "disappear" from these locations when iron intake is inadequate?
|
|
First, the iron stores get low. Second, iron is diminished in the plasma and you have low levels of circulating iron. Last, Iron begins to be missing from the red blood cells and you have iron deficiency anemia - sick red blood cells.
|
| |
Symptoms of Iron deficiency anemia
|
|
Fatigue and weakness
Cannot maintain body temperature
Change in mental/emotional state
Prone to infection
Adverse pregnancy outcomes
Impaired development
Pica? Ice crunch craving
|
| |
Groups at most risk for Iron deficiency anemia?
|
|
Infants, children, adolescents
Women of reproductive age
Pregnant women
Athletes
|
| |
Iron toxicity: acute v. chronic
|
|
Acute toxicity
Ingestion of a single large dose at one time
Chronic toxicity
*Caused by iron overload
*Most common cause is hemochromatosis
*Overconsumption of iron supplements or diet high in absorbable iron can increase iron stores
*Excess free iron promotes formation of free radicals and causes cell damage
|
| |
Iron deficiency and iron excess damage ______________
and _____________ _____ in rats.
|
|
Iron deficiency and iron excess damage mitochondria
and mitochondrial DNA in rats. |
| |
Meeting Iron need: you must consider the TOTAL diet to avoid excess or under consumption:
Best sources: _______
Bioavailability from heme sources ___________
" from non-heme sources ____________
Bioavailability goes ______ with low iron status
non-heme iron absorption is _______ by vitamin C
Take ___________ is you are in an at risk group.
|
|
Best sources are red meats and organ meats (heme)
Bioavailability for heme sources: 15 to 35% (absorbed)
Bioavailability for nonheme sources:
spinach & rice: 1%,
beans and grains: 4 to 7%
(bioavailability unknown for most non-heme iron sources
Bioavailability ↑ with low iron status
Nonheme iron absorption enhanced by vitamin C
Supplements recommended for groups at risk
|
| |
RDA for IRON:
_______ for adult men and _________ for adult women
Vegetarians – ________ for adult men and _______ for adult women
Pregnancy –_______ , _____ for pregnant vegetarian
|
|
8 mg/day for adult men and 18 mg/day for adult women
Vegetarians – 14 mg/day for adult men and 33 mg/day for adult women
Pregnancy – 27 mg/day
50 mg/day for pregnant vegetarian
|
| |
ZINC
The most ______intracellular trace element
Involved in functions of over 300 _____
Important for _____ and repair of ______ |
|
The most abundant intracellular trace element
Involved in functions of over 300 enzymes
Important for growth and repair of tissue |
| |
|
Zinc from _________ _____ is better absorbed because zinc in plant sources is often bound by ________ |
|
Zinc from animal food is better absorbed because zinc in plant sources is often bound by phytates
|
| |
Function
Enzyme ______
Synthesis of ______
Toxicity
Interferes with _____ metabolism
__ symptoms
|
|
Function
Enzyme cofactor
Synthesis of DNA/RNA
Toxicity
Interferes with copper metabolism
GI symptoms
|
| |
Zinc Deficiency =
|
|
Poor growth
Inadequate sexual development
Most common in underdeveloped countries
|
| |
3 Sources of Zinc
|
|
Animal products
Fortified cereals
Legumes
|
| |
Zinc RDA: Men, women and vegetarians?
|
|
11 mg/day for men
8 mg/day for women (11 mg/day during pregnancy)
Vegetarians – require ~ 50% more
|
| |
Iodine function:
|
|
Main component of Thyroid hormones
Regulates growth and metabolism |
| |
Iodine deficiency causes _____ and ______.
Iodine deficiency is the most well documented ____ deficiency.
|
|
Goiter- enlargement of thyroid
Cretinism- stunting of fetal growth and mental development
Most well documented causal deficiency
|
| |
Source of iodine?
|
|
Major source = Iodized salt
Also found in seafood and
Foods grown in soil with adequate iodine
|
| |
Other minerals which function as cofactors are:
(these are important minerals, but we don't have to know all about them - mostly just that they matter).
|
|
Copper (Legumes, whole grains, nuts, shellfish, seeds)
Chromium (Egg yolks, whole grains)
Manganese (Nuts, oats, legumes)
Molybdenum (Legumes, grains, nuts)
Selenium (Meat, fish, whole grains and plant sources - grown in selenium rich soil)
|
| |
Fluoride: function and deficiency?
|
|
Function
Reduces acid production by mouth bacteria
Improves tooth and bone strength
Deficiency
Tooth decay
|
| |
Toxicities in:
Fluoride (3x RDA)
Tooth ______ during development
Calcium (2x RDA)
Kidney _____, calcification of _______
Iron (>>3x RDA; UL = 45 mg)
__ upset, ____ damage
Zinc (4-5x RDA)
Reduced _________ absorption
Selenium (7x RDA)
Hair ____, nausea, _____
|
|
Fluoride (3x RDA)
Tooth mottling during development
Calcium (2x RDA)
Kidney stones, calcification of tissues
Iron (>>3x RDA; UL = 45 mg)
GI upset, liver damage
Zinc (4-5x RDA)
Reduced copper absorption
Selenium (7x RDA)
Hair loss, nausea, vomiting
|
| |
4 Contaminant Minerals:
Their sources?
|
|
Lead (Pb)
Cadmium (Cd)
Mercury (Hg)
Arsenic (As)
Often in nonfood sources, environmental contamination (water), fish and other marine food
|
| |
Supplements are ____ necessary if you are consuming a balanced diet. What four situation are the recommended in?
|
|
Vegan
Pregnancy
Food allergy/intolerance
Low kcal intake (esp elderly)
|
| |
The bioavialability of supplements may be poor because of these two factors:
Also, this type of dose may be harmful:
|
|
Vitamin-vitamin interactions
Mineral-mineral interactions
Megadose
|
| |
In General:*
________ increases blood pressure ( _____ retention leads to increased blood volume
_________ lowers blood pressure
|
|
In General:*
Sodium increases blood pressure (Fluid retention leads to increased blood volume)
Potassium lowers blood pressure
|
| |
Name one mineral present in the following hamburger components:
Whole wheat bun
Romaine lettuce (dark green leaf)
Tomato
Cheese
Ground beef patty
|
|
Whole wheat bun
Romaine lettuce (dark green leaf)
Tomato
Cheese
Ground beef patty |
| |
Which minerals are major minerals?
Which mineral is most abundant in the body?
Which minerals function in/as…
*Fluid balance?
*Structure?
*Blood components?
*Energy metabolism?
*Antioxidants?
|
|
outta time...
|
| |
What are good sources of…
Iron
Calcium
Sulfur
Magnesium
Zinc
Iodide
Sodium
Chloride
Potassium |
|
outta time...
|
| |
